Adrenal myelolipomas are rare, benign and usually asymptomatic tumors of the adrenal gland characterized by the predominance of mature adipocytes.
On imaging, they usually present as large masses with a variable amount of fat-containing components.
On this page:
Epidemiology
Myelolipomas are rare tumors of the adrenal glands with an estimated autopsy prevalence of 0.1-0.2%. They are usually identified in adults, either incidentally or if complicated by hemorrhage (see below). There is no gender predilection 9.
Associations
10% of patients with adrenal myelolipoma have congenital adrenal hyperplasia 20
Clinical presentation
Most lesions are asymptomatic 6 and may be discovered incidentally when the region is imaged for other reasons (i.e. an incidentaloma). Larger lesions (typically over 4 cm in size) can present with an acute retroperitoneal hemorrhage, and still others (especially when very large) with vague mass-related symptoms 9. There may be a right-sided predilection 5.
Although the tumor itself is non-functioning there is a relatively high incidence (10%) of associated endocrine disorders 9:
congenital adrenal hyperplasia (21-hydroxylase deficiency)
Conn syndrome (primary hyperaldosteronism)
rarely it can present in extra-adrenal locations 16
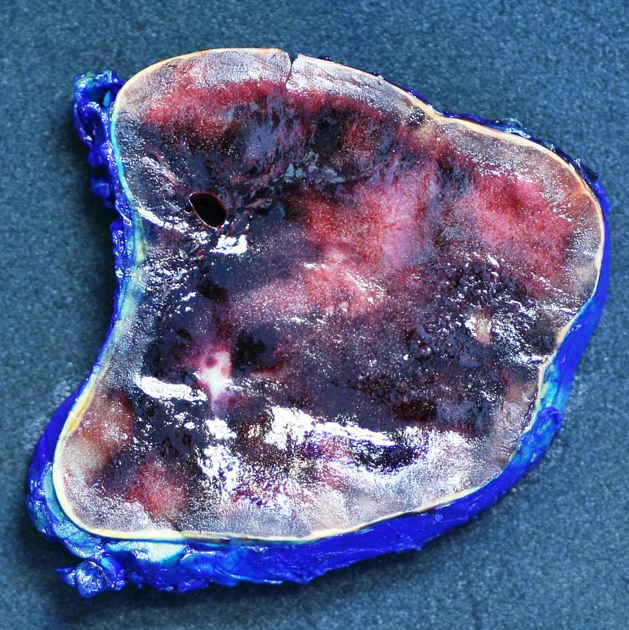
Pathology
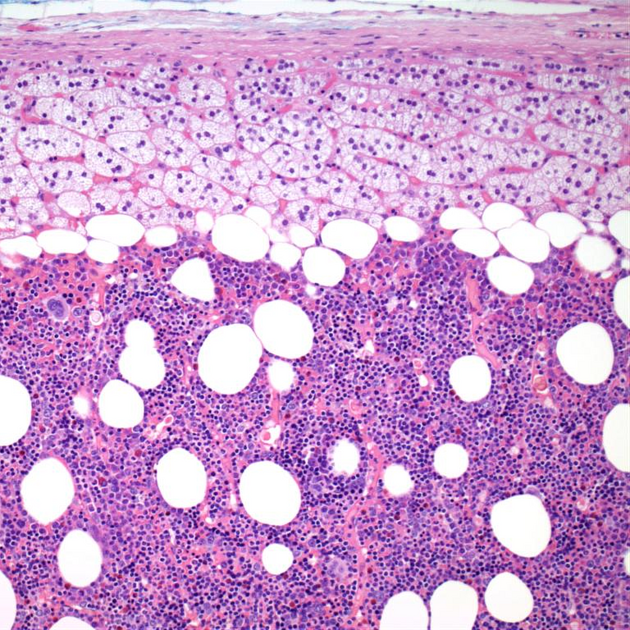
Histological examination demonstrates variable amounts of:
mature adipocytes (with distended lipid vacuoles) similar to bone marrow
hematopoietic cells (including cells from myeloid, erythroid and megakaryocytic cell lines)
The fatty component is often the predominant feature and therefore the most characteristic feature on imaging. The lesions can infrequently contain bone 10 or show partial replacement by hemorrhage or fibrosis.
Radiographic features
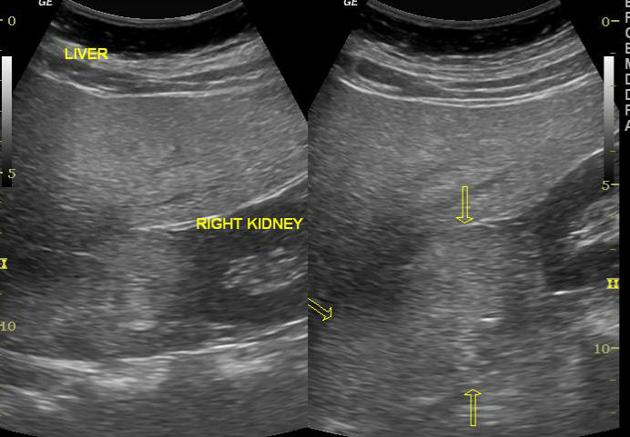
Ultrasound
Exact sonographic appearances are varied depending on individual tumor components 1. Usually is seen as a heterogeneous mass of mixed hyper- and hypoechoic components with the former primarily resulting from fatty portions. Areas of hemorrhage appear hypoechoic on ultrasonography 19. Fat within a myelolipoma can slow the ultrasound waves, resulting in the artifactual appearance of a discontinuous diaphragm 21.
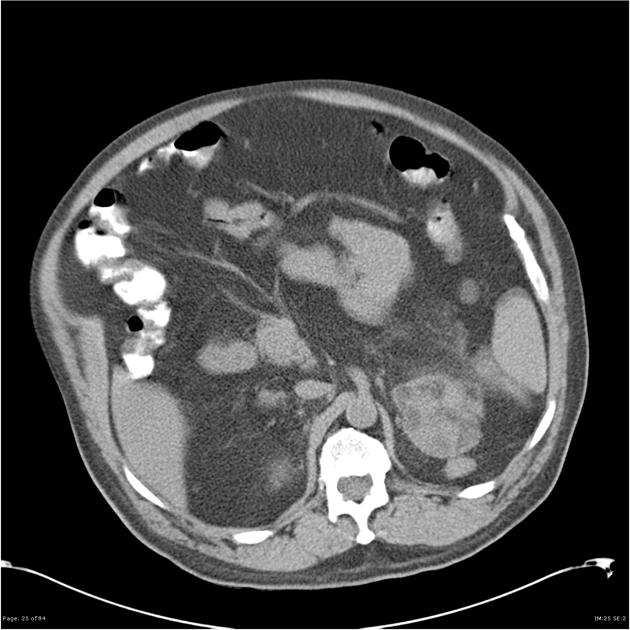
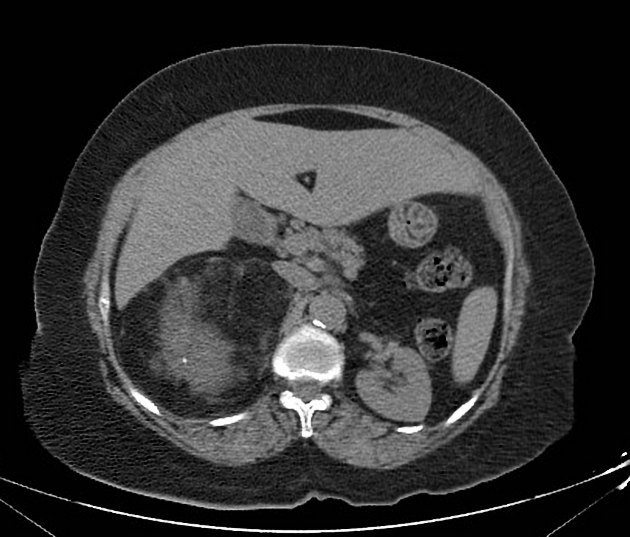
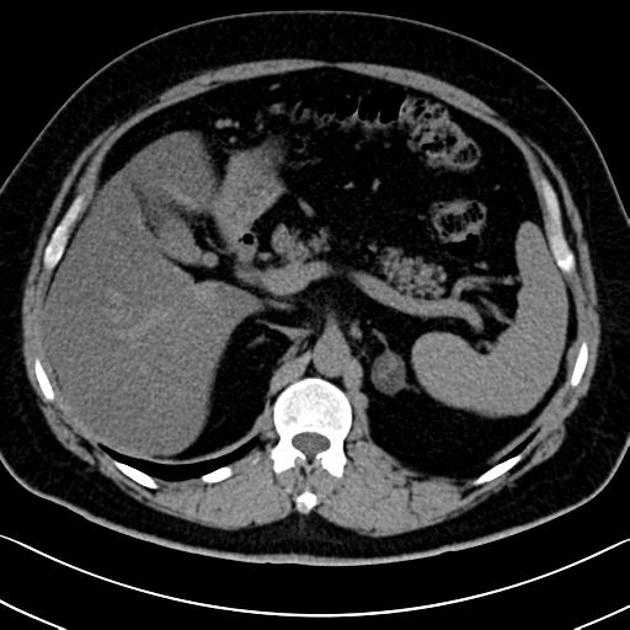
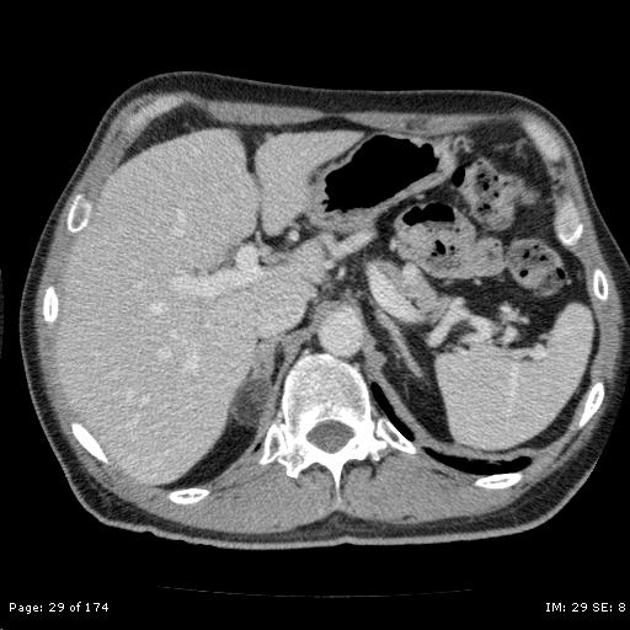
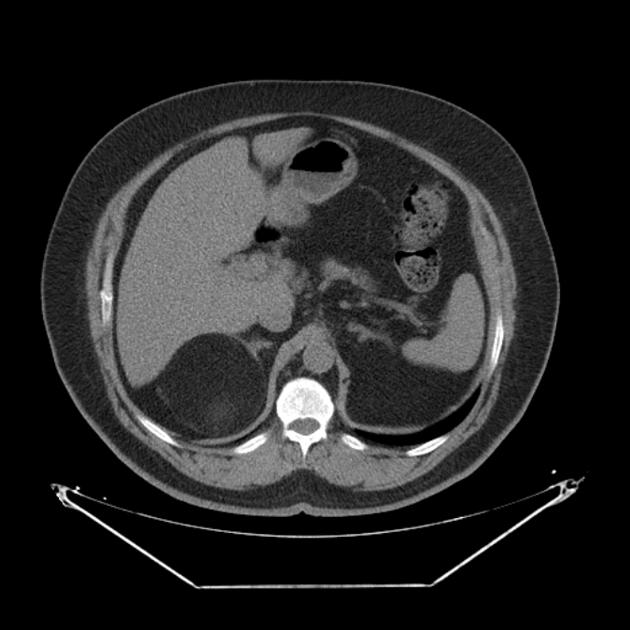
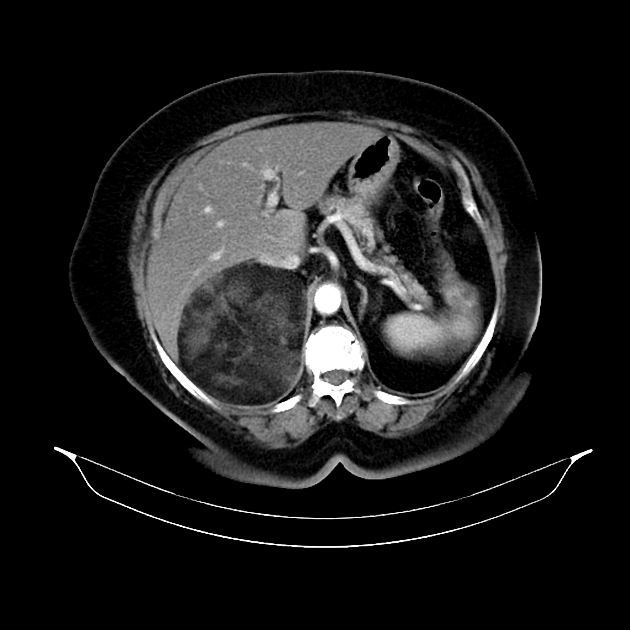
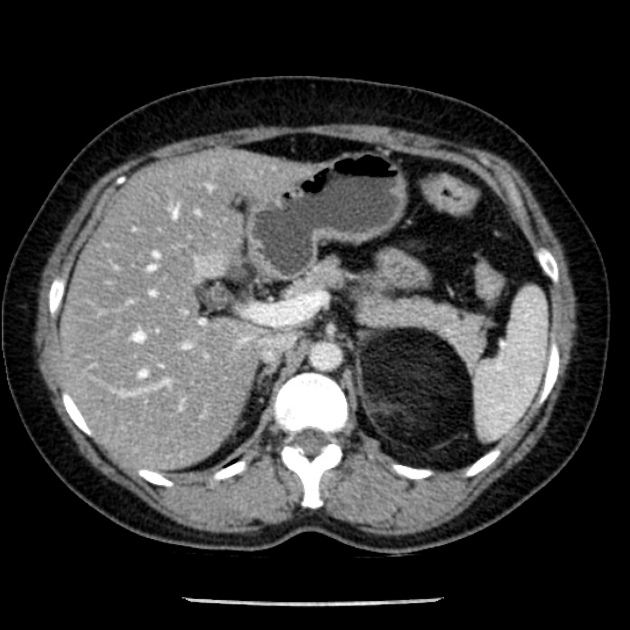
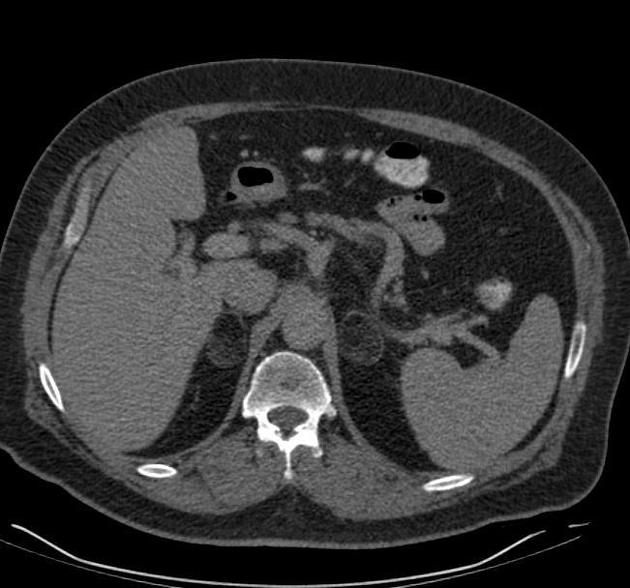
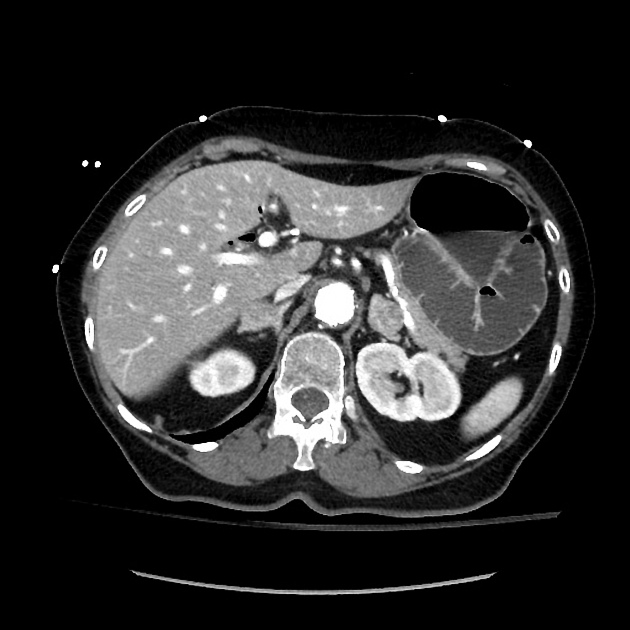
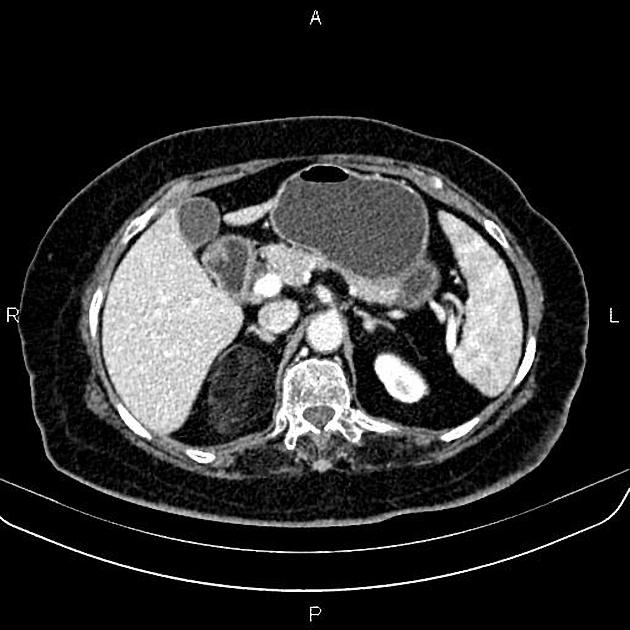
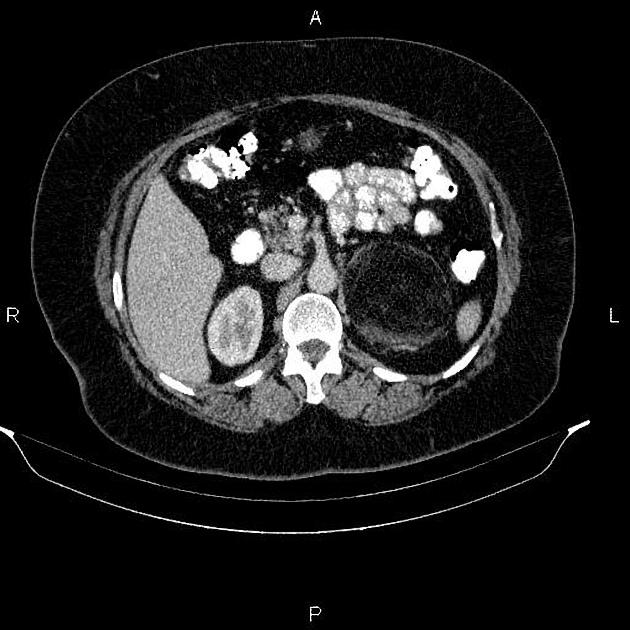
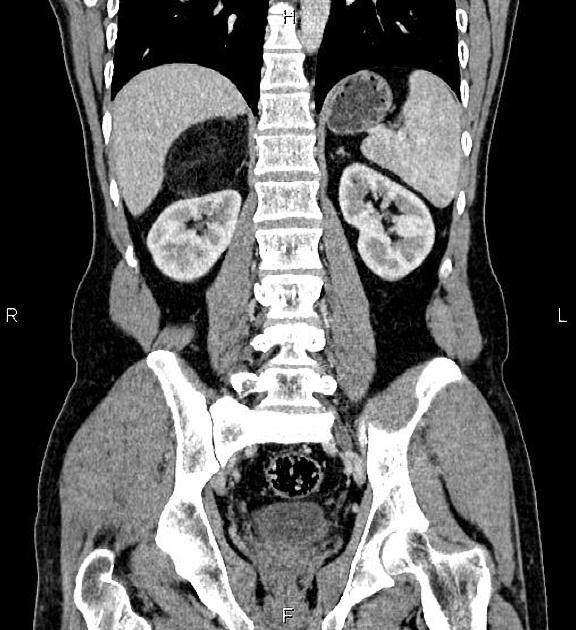
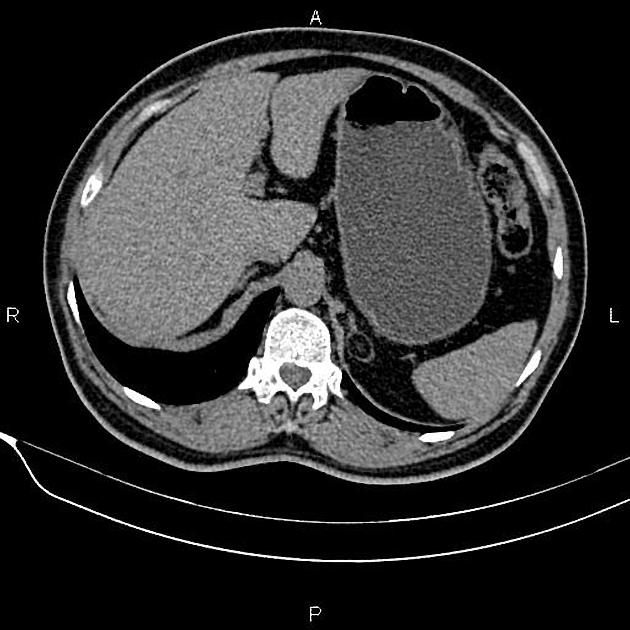
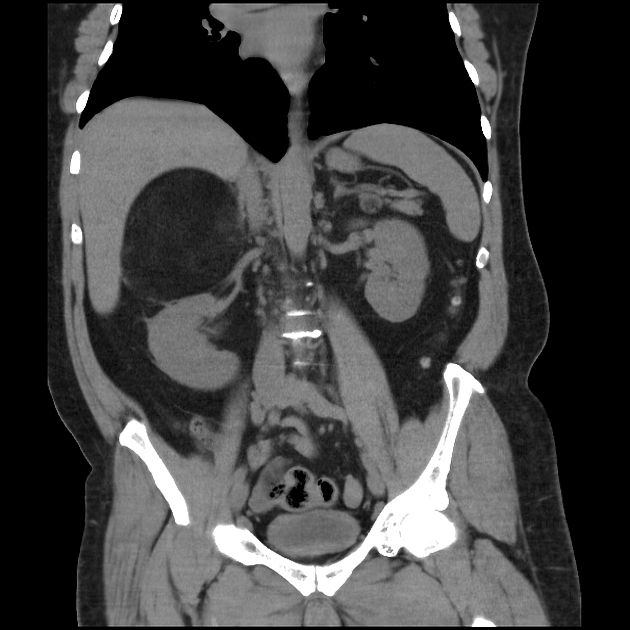
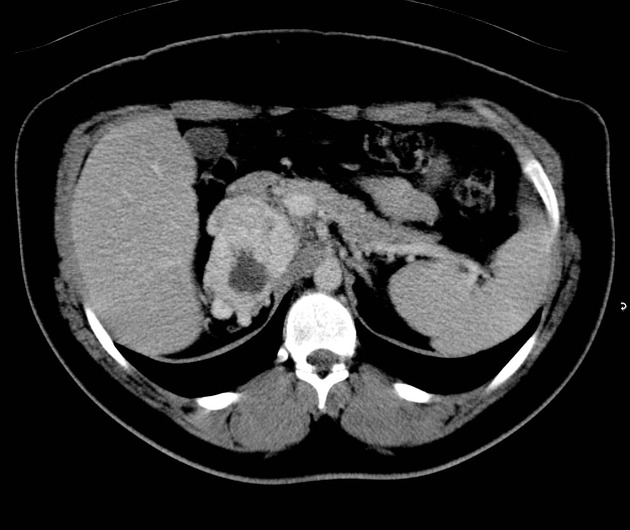
CT
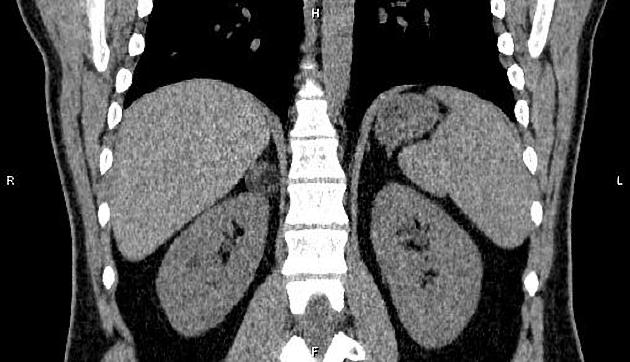
The CT appearance is usually characteristic. The typical adrenal myelolipoma appears as an adrenal lesion with fat-containing components. The mass is usually relatively well circumscribed, however masses that are mostly fat may be difficult to separate from surrounding retroperitoneal fat.
The amount of fatty component is variable, ranging from only a few small regions in an otherwise mostly soft tissue density mass (10%) to masses made up of roughly equal components of fat and soft tissue (50%) or almost completely composed of fatty tissue (40%) 9. The soft tissue and fatty components can be sufficiently mixed in some cases to render the mass a density similar to fluid.
Small punctate calcifications may be seen in 25-30% of cases 4,9.
If hemorrhage is present then regions of higher attenuation may be seen. This is more frequently seen in large lesions (>10 cm) 3.
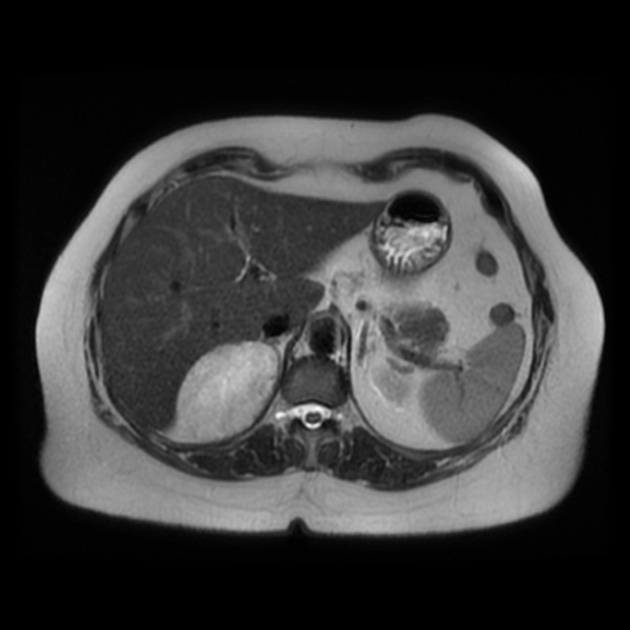
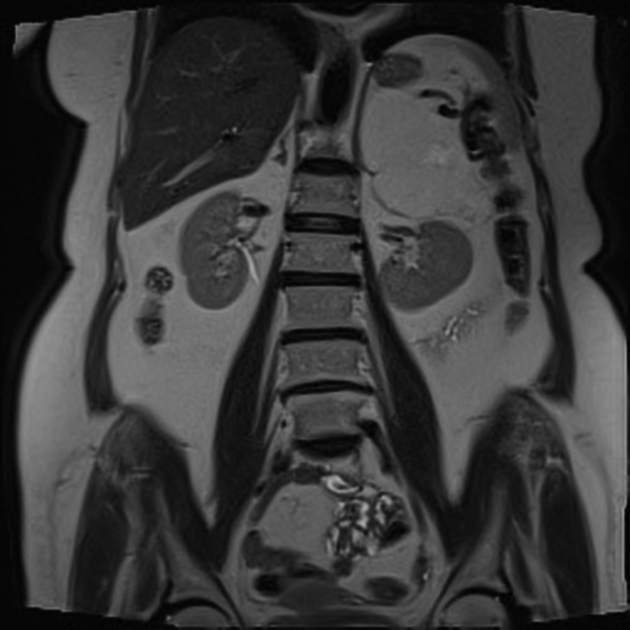
MRI
T1: typically hyperintense due to fat contents
T1 (FS): typically shows fat suppression
T2: generally intermediate to hyperintense but can sometimes vary depending on contents (especially blood products)
T1 C+ (Gd): shows striking enhancement 1
in and out of phase: in masses with mixed components, out of phase imaging may demonstrate signal loss as the microscopic fat cells usually have little intracellular water 9,11
Nuclear medicine
Adrenal myelolipomas typically do not demonstrate avid FDG uptake and it is generally lower than that of the liver background. However, in rare cases the adenomatous and hematopoietic elements can show an increased FDG uptake 12,13.
Treatment and prognosis
Adrenal myelolipomas are benign lesions with no recognized malignant potential 5. As such, if imaging features are characteristic and the lesion is small, no treatment is required.
If imaging findings are indeterminate, percutaneous biopsy can be performed. In larger lesions or where hemorrhage has occurred surgical excision is curative.
History and etymology
Adrenal myelolipomas were initially described by the German pathologist Edgar von Gierke (1877-1945) 6,22 in 1905, with the term myelolipoma coined by the French pathologist Charles Obenling (1895-1960) in 1929 7,17,18. Edgar von Gierke more memorably discovered glycogen storage disease type I, also known as von Gierke disease 22.
Differential diagnosis
General imaging differential considerations include:
fat-containing adrenocortical carcinoma
lipid-rich adrenal adenoma
adrenal teratoma: extremely rare
-
CT coronal reconstruction or MRI can help in determining the kidney as the origin of the lesion
adrenal lipoma: very rare
Practical points
when an adrenal lesion contains ≥50% macroscopic fat, the diagnosis of myelolipoma can be made with confidence 15












 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.