Autosplenectomy denotes spontaneous infarction of the spleen with resulting hyposplenism.
On this page:
Epidemiology
Autosplenectomy is most frequently encountered in patients with homozygous sickle cell disease, although it has also been reported in pneumococcal septicemia 1, and systemic lupus erythematosus 2. The demographics thus match those of sickle cell disease, usually occurring gradually in childhood with complete autosplenectomy achieved by the age of 8 4.
Clinical presentation
Clinically, patients may be asymptomatic accruing gradual damage, or more commonly present with repeated episodes of acute left upper quadrant pain due to splenic infarction. Pain may be referred via the diaphragm to the shoulder.
Pathology
The spleen is susceptible to repeated episodes of focal veno-occlusive disease with infarction resulting in gradual perivascular fibrosis and shrinkage of the organ.
Subtypes
Radiographic features
As the spleen infarcts, it shrinks and calcifies, becoming as little as 1 cm in diameter 6.
Plain film
If heavily calcified, the splenic remnant may be visible in the left upper quadrant.
Ultrasound
Ultrasound will either not be able to demonstrate a spleen at all, or identify a small irregular and shadowing nodule in the splenic bed.
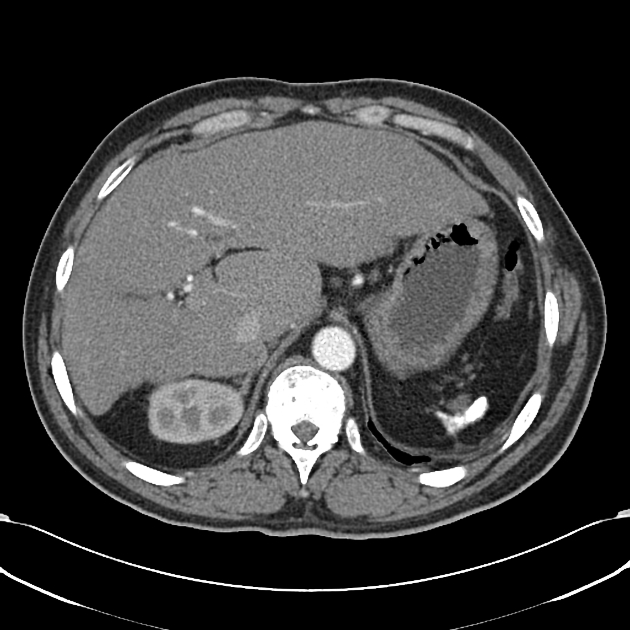
CT
CT easily identifies the abnormally small and irregular splenic remnant, which is usually calcified.
Nuclear medicine
Technetium-99m liver-spleen scans fail to demonstrate any splenic uptake.
Treatment and prognosis
The absence of a spleen leads to a number of hematological changes, the most important being that of a predisposition to overwhelming sepsis from encapsulated organisms including Pneumococcus and Haemophilus influenzae.
Prophylactic administration of penicillin has significantly reduced the incidence of infant and early childhood mortality from such infection 3.
Differential diagnosis
- surgical splenectomy
- hemosiderosis
- Thorotrast (thorium dioxide) accumulation: usually both the liver and lymph nodes are also affected
- wandering spleen







 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.