Ecchordosis physaliphora is a congenital benign hamartomatous lesion derived from notochord remnants, usually located in the retroclival prepontine region, but can be found anywhere from the skull base to the sacrum.
On this page:
Terminology
There has been some controversy as to whether intradural chordoma and large ecchordosis physaliphora are different entities. Some authors (such as Wolfe et al.) proposed the name 'intradural chordoma' for all intradural notochordal remnant lesions 8. Others (such as Rodriguez et al.) proposed that all intradural notochordal remnant lesions should be called ecchordosis physaliphora, until chordoma are pathologically proven to arise from the intradural compartment 9. However, they are considered distinct pathologies with a common origin.
Clinical presentation
Unlike chordomas which are often symptomatic due to brainstem or cranial nerve compression, patients with ecchordosis physaliphora are usually asymptomatic. They are found in ~2% of autopsies 1. Due to delayed FLAIR-enhancement, they may be more conspicuous on delayed contrast-enhanced MRI of the inner ear and may be found as an incidental finding on MRI hydrops imaging of the inner ear, e.g. for Ménière's disease, as an intensely enhancing structure on delayed contrast-enhanced FLAIR 11.
Pathology
Ecchordosis physaliphora arise from remaining notochord cells along the axis of the spine after embryogenesis. Unfortunately, ecchordosis physaliphora and chordoma are histologically indistinguishable, other than by examining the margins, the latter demonstrating infiltrative growth.
Radiographic features
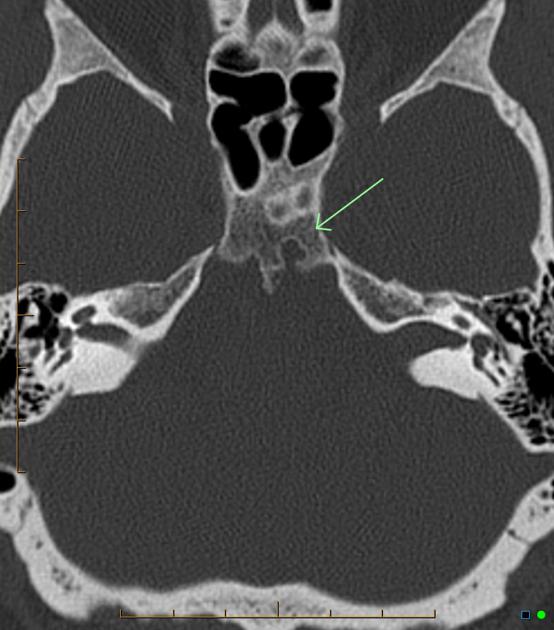
CT
CT is generally not sensitive for such lesions, mainly because of posterior fossa artifacts and the near CSF density of the mass. The bony clival defect is, however, visible as a well-demarcated smoothly corticated region, without aggressive features.
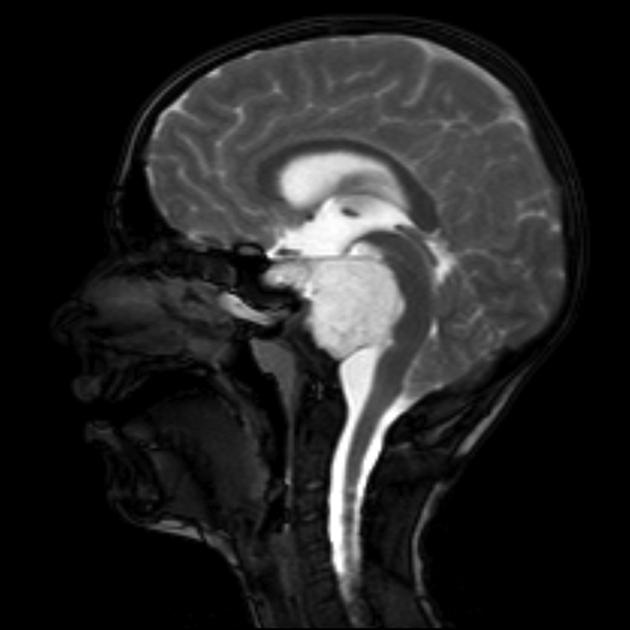
Occasionally an osseous stalk is seen at the base of the lesion which is said to be pathognomonic in this context 7.
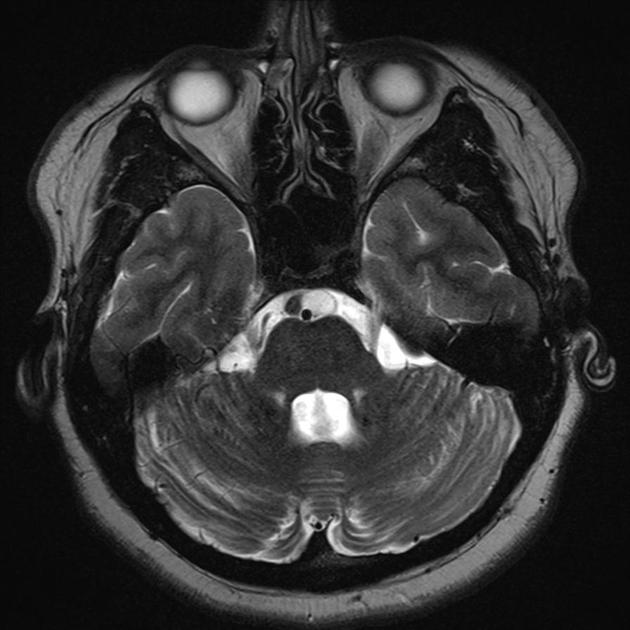
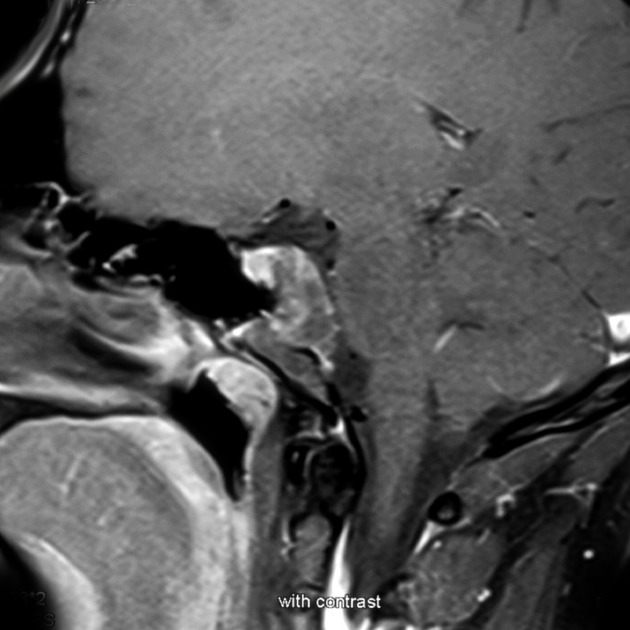
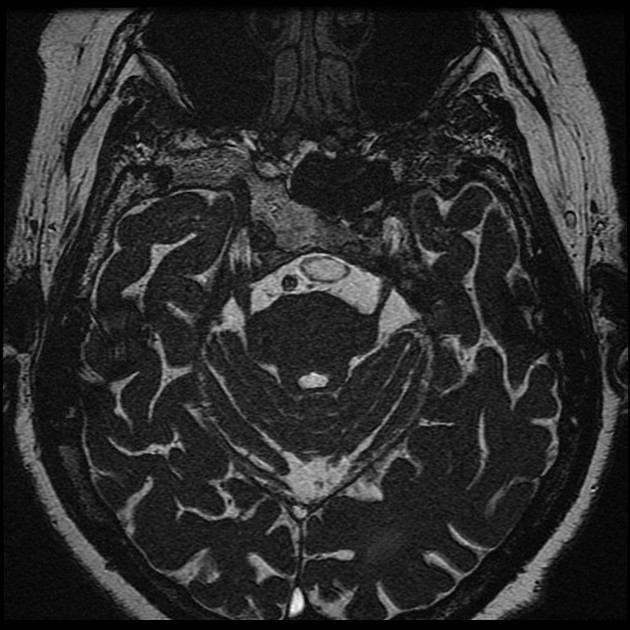
MRI
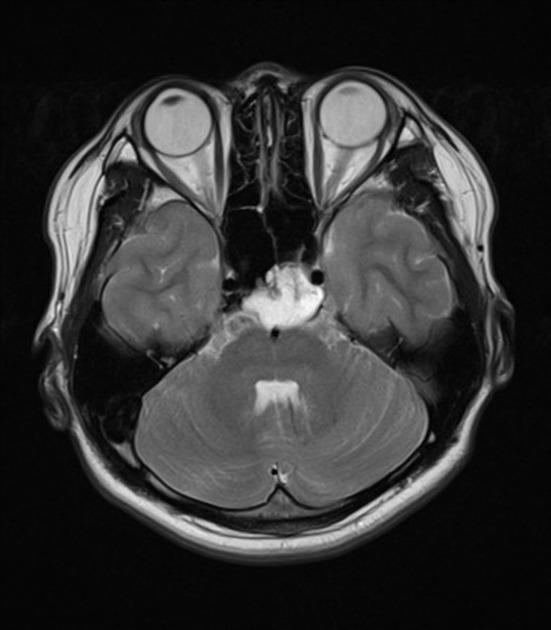
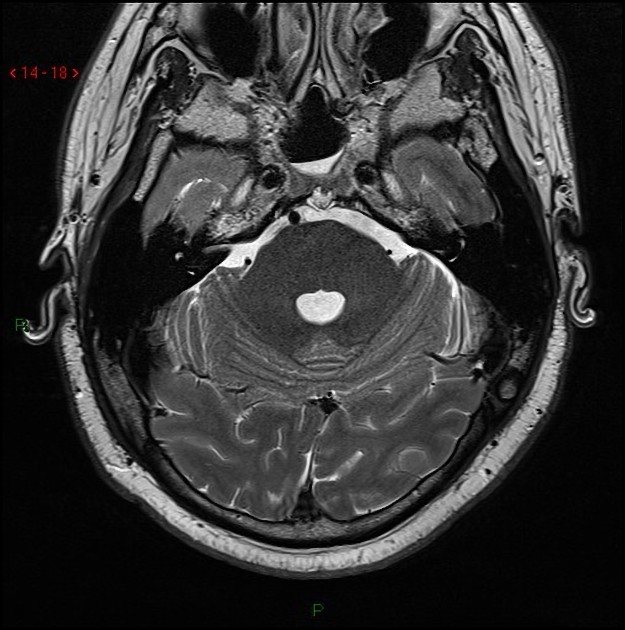
A stalk-like connection to the clivus is usually seen if high-resolution images are obtained.
Apart from the characteristic location (retroclival, prepontine, and intradural), MRI findings are non-specific, with signal similar to CSF:
T1: hypointense
T2: hyperintense
T1 C+ (Gd): no enhancement 1
FLAIR: may or may not suppress
Delayed FLAIR C+: enhancement 11
Care should be taken not to mistake delayed FLAIR enhancement for non-delayed T1 enhancement seen in most chordomas 11. Additionally, it can be challenging to identify on FLAIR due to the presence of flow artefact in the CSF of the pre-pontine cistern due to basilar artery pulsation.
History and etymology
Rudolf Virchow (1821-1902), a German physician and pathologist first described a similar lesion in 1857 and mistook it as a degenerative process affecting the spheno-occipital synchondrosis with cartilaginous components and termed it "ecchondrosis physaliphora" which comes from the Greek "chondros" meaning cartilage and "physalis" meaning bubble. Friedrich von Muller suggested a notochordal origin in 1858. In 1898 Ribbert confirmed its notochordal origin and coined the modern term of "ecchordosis physaliphora" 10.
Differential diagnosis
The differential diagnosis of retroclival intradural lesions consists mainly of 4:
chordoma: generally symptomatic and enhances after contrast administration
skull base metastasis
arachnoid cyst: communicates with subarachnoid space, follows CSF intensity pattern and no enhancement








 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.