Epiploic appendagitis is a rare self-limiting ischemic/inflammatory process that affects the appendices epiploicae of the colon and may either be primary or secondary to adjacent pathology. This article pertains to primary (spontaneous) epiploic appendagitis. The term, along with omental infarction, is grouped under the broader umbrella term intraperitoneal focal fat infarction 9.
On this page:
Epidemiology
This condition usually affects patients in their 2nd to 5th decades with a predilection for women and obese individuals, presumably due to larger appendages 6. Its frequency is approximately 1.3% of cases with abdominal pain and its incidence is around 8.8 cases per million per year 10.
Clinical presentation
Patients typically present with abdominal pain and guarding. It is essentially indistinguishable from diverticulitis and acute appendicitis (depending on location) and, although an uncommon condition, it accounts for up to 7% of cases of suspected diverticulitis 1. Since there is focal peritoneal irritation, pain may be more localized than with other causes of acute abdominal pain.
Pathology
Epiploic appendagitis merely denotes inflammation of one or more appendices epiploicae, which number 50-100 and are distributed along the large bowel with variable frequency 3,4,6:
rectosigmoid junction: 57%
ileocecal region: 26%
ascending colon: 9%
transverse colon: 6%
descending colon: 2%
The pathogenesis is thought to be due to torsion of a large and pedunculated appendage epiploica, or spontaneous thrombosis of the venous outflow, resulting in ischemia and necrosis 3.
Radiographic features
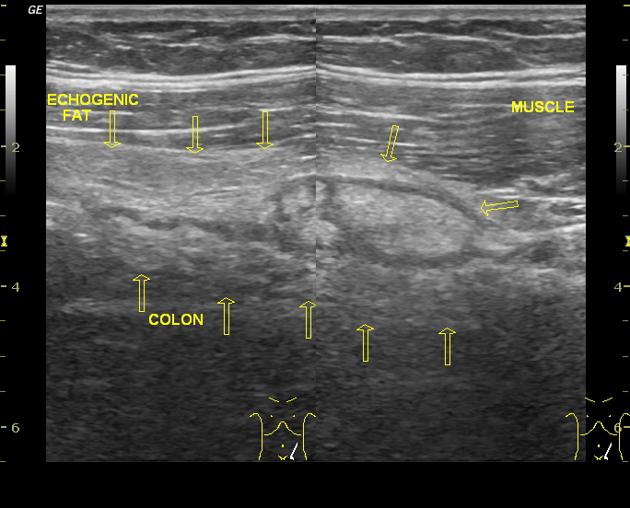
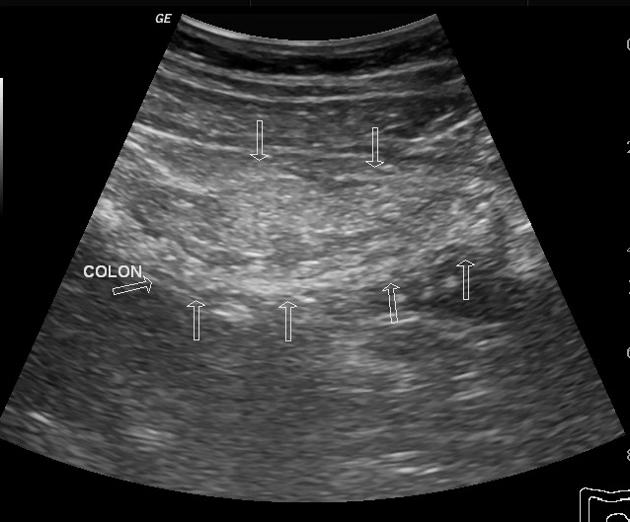
Ultrasound
Evaluation at the area of tenderness may show a rounded, non-compressible hyperechoic mass, without internal vascularity and surrounded by a subtle hypoechoic line. 5. They are typically 2-4 cm in maximal diameter.
They typically exert local mass effect but are not usually associated with bowel wall thickening or ascites 5.
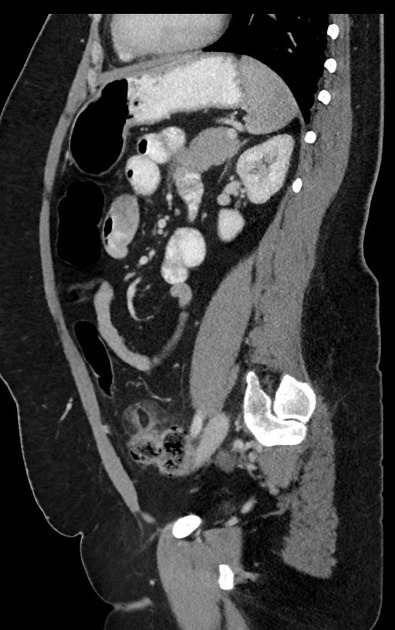
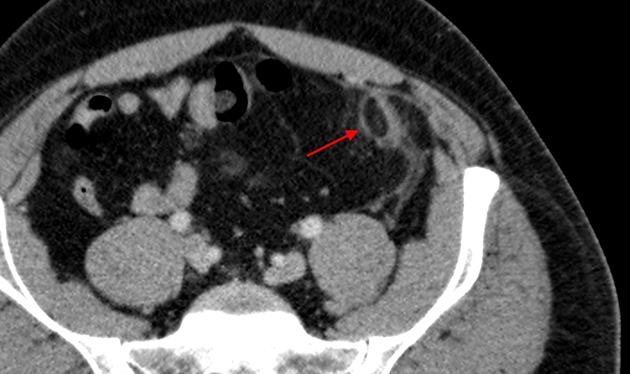
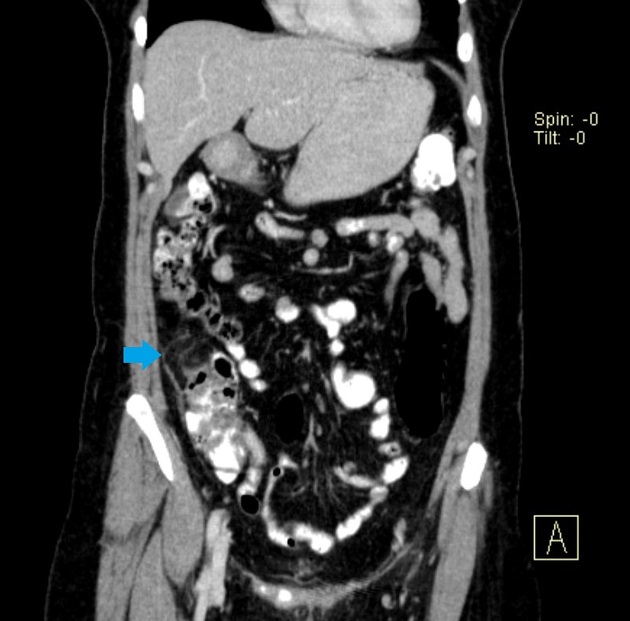
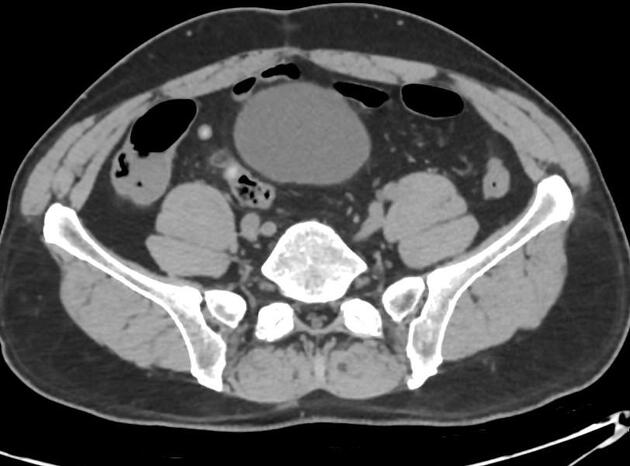
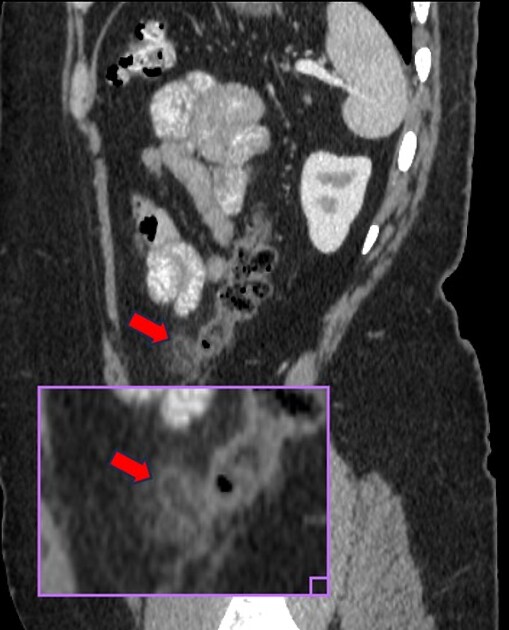
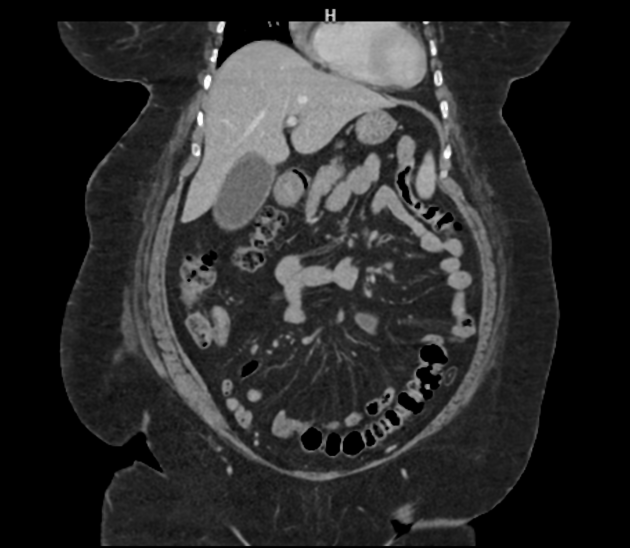
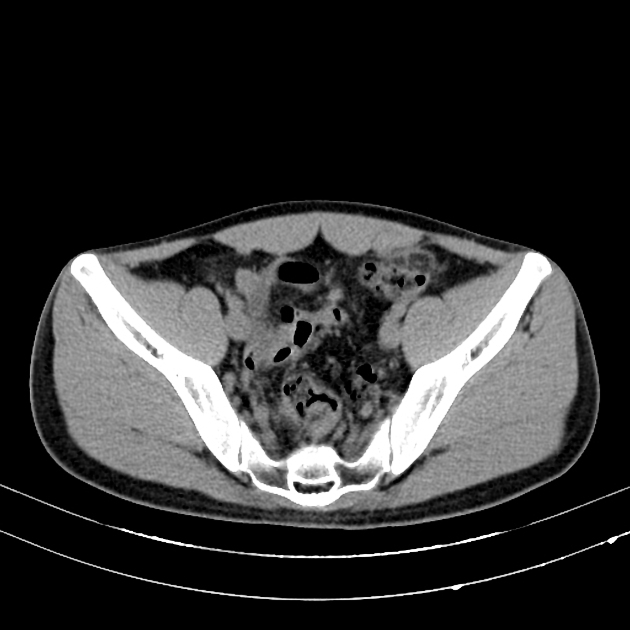
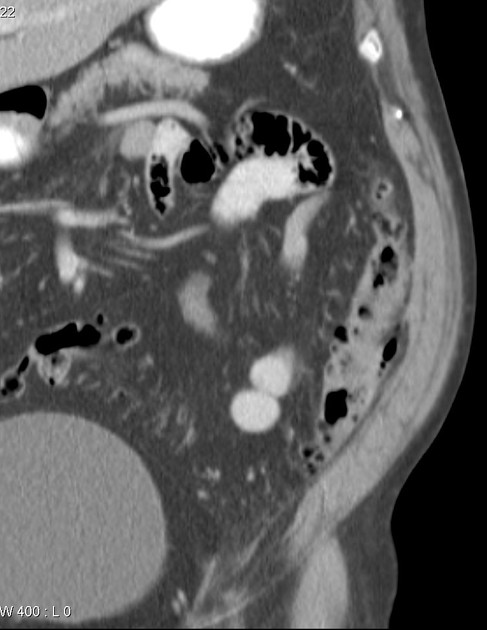
CT
The CT appearance is usually characteristic:
a fat-density ovoid structure adjacent to the colon, usually 1.5-3.5 cm in diameter 2
thin high-density rim, known as the hyperattenuating ring sign (1-3 mm thick) 5,6
surrounding inflammatory fat stranding, and thickening of the adjacent peritoneum
a central hyperdense dot (representing the thrombosed vascular pedicle) 6
adjacent colonic wall thickening is not usually associated, but if present is usually minimal and the amount of fat inflammation is out of proportion to colonic wall thickening
the inflamed appendage is classically located on the anterior aspect of the sigmoid or descending colon, but it may be located anywhere along the circumference of the colon
Chronically, an infarcted epiploic appendage may calcify and may detach to form an intraperitoneal loose body (peritoneal 'mice').
It may rarely involve the vermiform appendix epiploic appendages as so-called "epiploic appendagitis of the vermiform appendix" 8, mimicking appendicitis both clinically and potentially on CT.
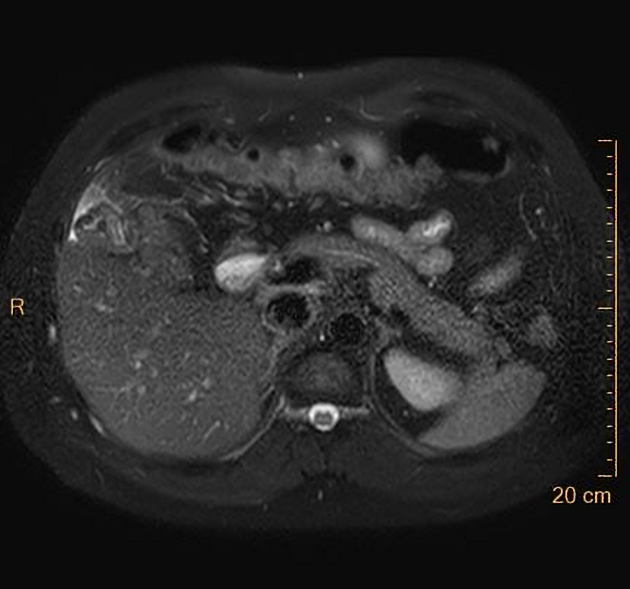
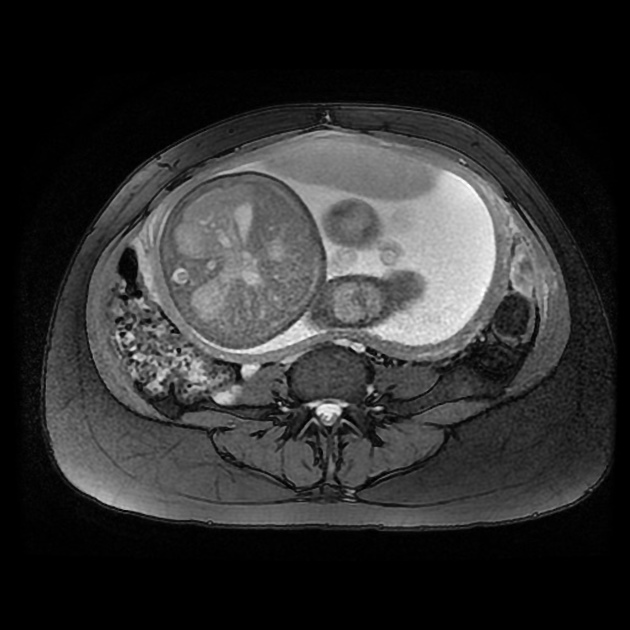
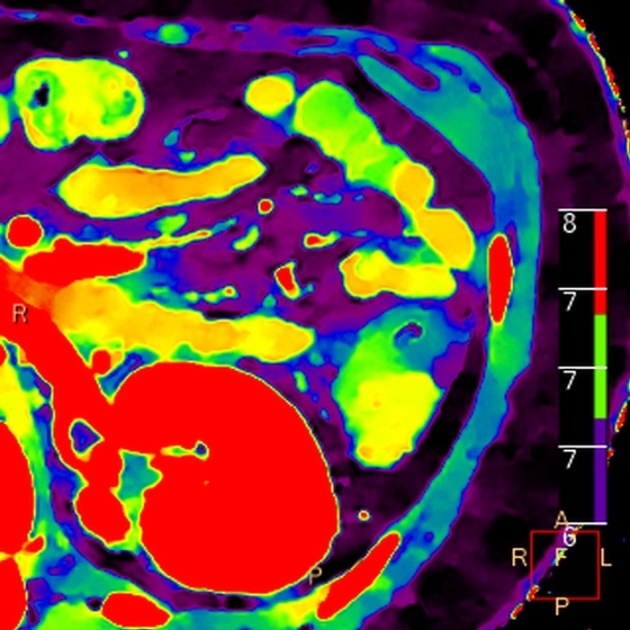
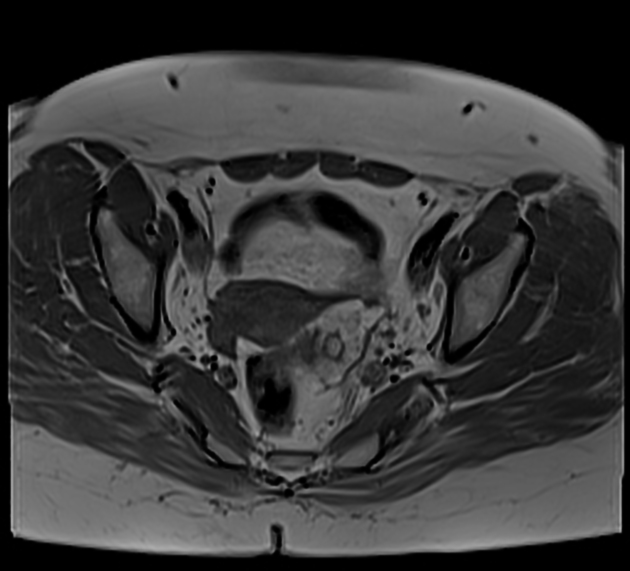
MRI
Although uncommonly used in a setting of acute abdominal pain, MRI features are also characteristic 6:
T1: often shows a rounded high signal mass with slightly reduced signal compared to normal fat, due to inflammatory stranding; hypointense 2-3 mm rim
T2: often seen as a high signal mass which attenuates on fat-suppressed sequences; hyperintense 2-3 mm rim with surrounding high signal stranding; central low signal vein
T1 C+ (Gd): shows vivid rim enhancement
Treatment and prognosis
Epiploic appendagitis is a self-limiting disease, and thus correct identification on CT prevents unnecessary surgery 2. Although it sometimes mimics acute abdominal diseases for which surgery is required, treatment options for epiploic appendagitis often do not include surgery; Management usually focuses on pain control with NSAID and observation.
History and etymology
Epiploic appendagitis was employed for the first time by Lynn et al. in 1956. The first CT description occurred in 1986 by Danielson et al. 2.
Differential diagnosis
Imaging differential considerations include:
acute appendicitis: if right-sided
omental neoplasms e.g. exophytic angiomyolipoma, atypical liposarcoma
omental infarction occurs close to ascending colon and is typically larger than 3 cm



















 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.