Intradural spinal mass lesions are relatively uncommon, compared to intracranial or extradural masses, and can be challenging to diagnose. Additionally, the need for a pre-operative/non-operative diagnosis is in many ways greater as biopsy of lesions within the cord has the potential of devastating neurological impairment. As such, a systematic approach to these lesions is required.
On this page:
Imaging options
MRI is the modality of choice for the assessment of lesions within the spinal canal as it has exquisite anatomical contrast and structural resolution, is able to image all compartments, and affords assessment for the presence of enhancement, cystic change, and blood products.
Myelography historically was of prime importance but is now done only in patients for whom an MRI is contraindicated (e.g. those fitted with a non-MRI-compatible/conditional pacemaker) or who could potentially have too much artifact from spinal instrumentation, or occasionally as a problem-solving technique (e.g. spinal arachnoid cyst vs ventral cord herniation). This is usually combined with CT (i.e. CT myelography).
CT remains the best modality to assess the osseous structures and is especially important in planning instrumentation, although this is usually not required for intradural tumors as the vertebral bodies are essentially unaffected in virtually all cases.
Angiography is useful in a select group of patients who have vascular lesions (for both vascular malformations and vascular tumors). Endovascular treatment may be useful in some instances.
Ultrasound, except in the infant, does not have a role in diagnosis, as it is unable to image the intradural compartment due to the overlying posterior spinal elements.
As such, the rest of this article focuses on MRI.
MRI protocol
A standard approach to imaging an intradural mass consists of:
T1 sagittal and axial
T2 sagittal and axial
T1 C+ sagittal and axial, with one or both planes fat-saturated (especially when there is foraminal extension or when there is concern for an extradural process)
Additional sequences may also be useful, including:
CSF flow studies
gradient echo sequences (for blood products/calcification)
high resolution
diffusion-weighted imaging
tractography
Normal appearance on MRI
The spinal cord is rostrally continuous with the medulla oblongata and extends caudally to the conus medullaris. In adults, the tip of the conus typically terminates at the level of L1-L2, however it may terminate as high as mid-T12 or as low as L2-L3. The cord has two enlargements, cervical (C4-T1) and lumbosacral (T11-L1). The cervical enlargement provides innervation to the upper limbs via the brachial plexus, while the lumbosacral enlargement innervates the lower limbs via the lumbosacral plexus.
The spinal nerve roots arising from the lumbosacral enlargement and conus medullaris comprise the cauda equina, which runs through the lumbar cistern. The filum terminale, a continuation of pia mater, descends from the tip of the conus within the lumbar cistern amid the nerve roots of the cauda equina. After it leaves the inferior end of the dural sac, it passes through the sacral hiatus to insert on the dorsal aspect of the coccyx.
The spinal dura mater is the outermost covering membrane of the spinal cord. Superiorly, it adheres to the margin of the foramen magnum where it is continuous with the cranial dura mater. Its caudal end most commonly occurs at the level of S2. The dura extends for a distance into the neural foramen along each nerve root. The dura is separated from the vertebrae by the epidural space, which contains fat and the epidural venous plexus.
The subdural space, between the dura and arachnoid layers, is a potential space, with the dura and arachnoid normally apposed to one another. The subarachnoid space, between the arachnoid mater and pia mater, is continuous with the intracranial subarachnoid space and contains cerebrospinal fluid. It extends a short distance along with the nerve roots into the neural exit foramina. The pia mater is applied to the surface of the spinal cord and the roots of the spinal nerves.
Axial MRI scans of the cord demonstrate the anterior median fissure, a prominent cleft in the midline of the ventral surface of the cord. The posterior median sulcus is a shallow indentation on the dorsal aspect of the cord. The ventral nerve roots exit the spinal cord at the anterolateral sulcus and the dorsal nerve roots enter the cord at the posterolateral sulcus. The dorsal intermediate sulcus separates the dorsal column into the gracile (more medial) and cuneate (more lateral) tracts.
Features of the internal structure of the spinal cord may be visualized on MRI. The central grey matter has a characteristic H-shape. The anterior grey columns are larger than the posterior grey columns. The anterior grey columns are separated from the ventral surface of the cord by the white matter of the anterior funiculus. The dorsal grey matter extends nearly to the surface of the cord. Smaller lateral horns are present from T1 to L2 and from S2 to S4. The central canal of the cord is located within the grey commissure. Although the normal central canal contains CSF and is lined by ependyma, it is often discontinuous in adults.
Systematic approach to interpretation
As with all studies, having a systematic approach to intradural lesions is essential if subtle lesions are to be detected and the differential adequately narrowed. There is no single correct way to do this, and what is presented is merely a personal approach.
Location
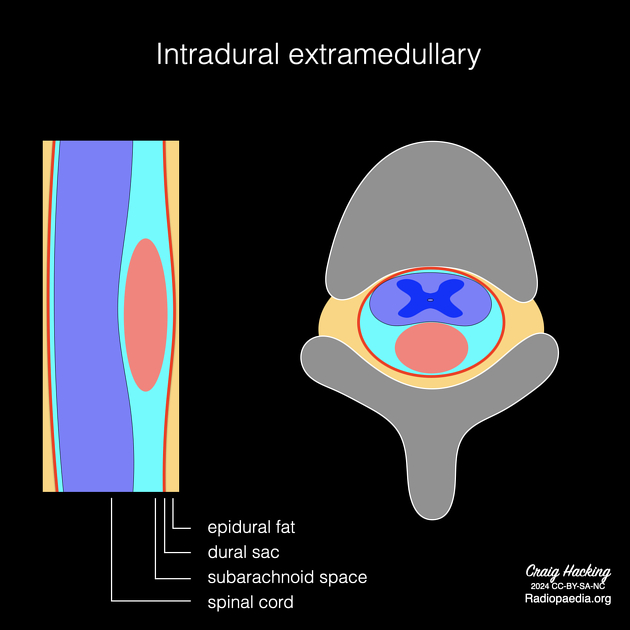
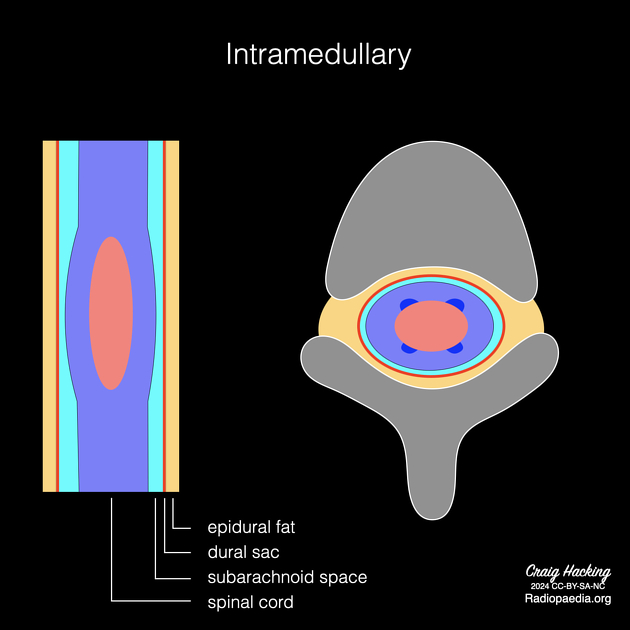
The relationship of the mass to the cord is of prime importance and typically two compartments are considered: intramedullary (i.e. within the cord), intradural extramedullary (i.e. within the theca but outside of the cord). Additionally, the cauda equina region is often considered separately as a number of lesions are particular to it. The vast majority of cases will then fall into a relatively small number of more common entities for each region (for a more complete list please refer to neoplasms of the spinal canal):
-
spinal astrocytoma (diffuse)
spinal cord metastasis (intramedullary)
Although in most cases which compartment a lesion is in is obvious, sometimes larger lesions can be challenging, and typically the questions which arise are:
Is this a large extramedullary mass compressing the cord or an exophytic intramedullary mass?
Is this a conus lesion or a lesion just below the conus?
In most cases a careful assessment not so much of the mass but of the cord immediately above or below the mass is helpful. An extramedullary mass will push the cord away from it whereas an intramedullary lesion will expand and thin the cord around it (this is known elsewhere as the claw sign).
Sometimes one must also consider whether a mass is actually extradural, and again examination of the dura above and below the mass is useful. Other than extension into the foramen as is seen in nerve sheath tumors and sometimes meningiomas (so-called dumbbell lesions), it is rare for intradural masses to extend into the extradural compartment, and thus vertebral body or clear epidural involvement usually means that the mass is extradural.
Intramedullary lesions
Once a lesion is determined to be within the cord substance, its location within the cord is important. Ependymomas, for example, are usually located centrally whereas astrocytomas are usually eccentric.
Intradural extramedullary lesions
Intradural extramedullary lesions may be related to nerve roots and may extend into the foramen (e.g. schwannomas and neurofibromas) or they may have a broad dural attachment (e.g. meningiomas) or be attached to the cord (leptomeningeal metastases).
Cauda equina / filum terminale lesions
It is sometimes possible, especially with smaller lesions, to identify whether or not it arises from the filum terminale (e.g. myxopapillary ependymoma) or from one of the nerve roots (e.g. schwannoma). The filum terminale is usually slightly thicker than nerve roots and may have a small amount of fat. If one carefully traces nerve roots from below, one can trace them rostrally on each side as paired structure, as they ascend through the sub-articular recesses.
Signal characteristics
T1
Most intradural tumors are isointense or hypointense on T1 weighted images. T1 hypointensity may also reflect hemorrhage, cyst formation, fibrous tissue and calcification. T1 hyperintensity may be present if the lesion is hemorrhagic or if it is a fat-containing mass such as a dermoid, teratoma, or lipoma. Melanin also results in T1 shortening, even in the absence of hemorrhage. Myxopapillary ependymomas are usually isointense, however, a prominent mucinous component occasionally results in T1 hyperintensity. Ganglioglioma typically demonstrates mixed signal intensity on T1 weighted images. This is due to the dual cellular elements of the tumor (ganglion cells and glial elements) and is a unique finding among spinal cord tumors.
T2
Spinal cord tumors are usually hyperintense on T2 weighted images. An exception is solitary fibrous tumors which are markedly hypointense on T2 weighted studies. The T2 hypointensity of these tumors is thought to be due to the presence of abundant collagen fibers. Tumor hemorrhage leads to a hypointense hemosiderin rim on T2 weighted images (“cap sign”). This sign is suggestive of but not pathognomonic for ependymoma. T2 hypointensity may also reflect tumor calcification.
Peritumoural edema manifests as T2 hyperintensity surrounding the tumor nodule. Although this is a nonspecific finding, extensive edema, which is disproportionate to the size of the mass, is typical of a metastasis.
Care should be taken to assess for the presence of prominent vascular flow voids, which may either indicate a vascular tumor (e.g. hemangioblastoma) or a vascular malformation (e.g. spinal dural arteriovenous fistula).
Contrast enhancement
Most spinal neoplasms demonstrate contrast enhancement, although the pattern of enhancement is highly variable. Lack of enhancement, however, certainly does not exclude a neoplasm as a minority of tumors do not enhance at all. Conversely, intradural lesions that mimic spinal neoplasms may demonstrate variable contrast enhancement. Such lesions include cavernous malformations, dural arteriovenous fistulas, spinal cord infarction, demyelinating lesions, transverse myelitis, and spinal cord abscesses.
Blood products
Depending on age, blood products have a variable appearance on MRI (see aging blood on MRI). Chronic blood appears hypointense on T1 and T2 weighted images and demonstrates blooming on susceptibility-weighted images. Hemorrhage within a spinal tumor suggests ependymoma, hemangioblastoma, paraganglioma, or a hemorrhagic metastasis (thyroid, melanoma). Cavernomas and cord contusions also demonstrate blood products of varying ages.
Multiplicity
Depending on the likely diagnosis, examination of the rest of the neuraxis may be required and is recommended especially when appearances suggest leptomeningeal metastases or ependymoma. Similarly, the presence of multiple lesions (e.g. spinal nerve sheath tumors) may raise concern for a phakomatosis (e.g. NF1 or NF2).
Radiology report
If an intradural spinal mass is identified, the following features should be described, as they may help narrow the differential diagnosis or have clinical implications:
size
signal intensity on T1 and T2 weighted images +/- appearance on other sequences
presence and pattern of contrast enhancement
-
location
intramedullary or intradural extramedullary
spinal cord segment(s) affected (see below)
for intramedullary tumors, location within the spinal cord (central vs eccentric)
exophytic component
single vs multiple lesions
presence of: hemorrhage, calcification, necrosis
associated cysts (tumoral, non-tumoral) or syringomyelia
-
surrounding abnormalities
peritumoural edema
prominent flow voids
leptomeningeal enhancement
bony changes (though these are relatively rare) - widening of the spinal canal, scalloping of the posterior vertebral bodies, neural exit foraminal enlargement, scoliosis
compression of the spinal cord or displacement of nerve roots
Spinal level nomenclature
Although anatomy textbooks always describe standard 7 cervical, 12 thoracic, and 5 lumbar vertebrae, in reality, some degree of variation on this general layout is present in a significant number of patients. For example, a lumbosacral transitional vertebra (LSTV) is a common variant (with L5 sacralization being more common than S1 lumbarization), or, much less commonly, an additional pair of ribs can be present. Such variation results in the potentially discrepant numbering of levels, depending on interpretation and whether the levels are counted from above or below.
It is thus essential that in all cases where anatomy is a variant, a pedantic, careful, and explicit description of the method the levels have been numbered be included in the report.



 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.