Tectal glioma
Updates to Article Attributes
Tectal gliomas fall under the grouping of childhood brainstem gliomas and unlike the other tumours in that group they are typically low grade astrocytomas with good prognosis.
Epidemiology
Tectal plate gliomas are encountered in children and adolescents 4. A male predilection has sometimes been reported although this is by no means certain 3.
An association with neurofibromatosis type I (NF1) has been reported 3-4.
Clinical presentation
Their expansion within the brainstem causes narrowing the aqueduct of Sylvius and causing obstructive hydrocephalus with presentation usually secondary to headache 3-4.
Additional symptoms may include gaze palsies, due to compression of the medial longitudinal fasiculusfasciculus leading to an upgaze paslypalsy, diplopia or Parinaud syndrome, although these are uncommon 3-4.
Pathology
The vast majority of lesions are low grade astrocytoma, although occasionally other glial series tumours are encountered in the tectal region including ependymoma, ganglioglioma and primitive neuroectodermal tumours (PNET) 3.
Radiographic features
CT
Typical CT finding is homogenoushomogeneous expansion of tectal plate, isodense to grey matter with minimal enhancement inon postcontrast images 1,3.
On On CT it is not uncommon to find a central tectal calcification 2-3.
MRI
Typically the tumours demonstrate expansion of the tectal plate by a solid nodule of tissetissue.
-
T1:
- isoiso to slightly hypointense to grey matter 1-3 -
T2:
- hyperintensehyperintense to grey matter -
T1 C+ (Gd):
: usuallyusually no enhancement
With time the mass can develop small cystic spaces (sometimes associated with neurological deficits) or calcification 3.
Higher grade tumours tend to be larger and tend to enhance more vividly 3.
Treatment and prognosis
As tectal plate gliomas are low grade and often very slow growing, shunting is often the only required intervention for long term survival. As surgical biopsy can have significant morbidity in this area, usually the diagnosis is made on imaging findings alone.
In the minority of patients who progress, radiotherapy often leads to local control or even tumour regression 2. Surgical excision is sometimes necessary 3.
Imaging predictors of patients who will need further treatment include a size greater than 2.5cm.5 cm and presence of contrast enhancement 3.
Differential diagnosis
When the tectum is near-normal then the differential is largely limited to:
-
aqueductal stenosis
- no mass lesion
- a focal stenosis or web may be visible
With larger lesions, where the mass is not definitely arising from the tectal plate then the differential is essentially that of a pineal region mass and therefore includes:
- pineal parenchymal tumours and germ cell tumours
- pineal cyst
- meningioma
- cerebral metastasis
- cavernous malformation
In patients with NF1 a hamartoma should also be considered. They tend to have some T1 hyperintensity 4.
-<p><strong>Tectal gliomas</strong> fall under the grouping of childhood <a title="Brainstem glioma" href="/articles/brainstem-glioma">brainstem gliomas</a> and unlike the other tumours in that group they are typically low grade <a title="Astrocytoma" href="/articles/astrocytoma">astrocytomas</a> with good prognosis. </p>-<h4>Epidemiology</h4>-<p>Tectal plate gliomas are encountered in children and adolescents <sup>4</sup>. A male predilection has sometimes been reported although this is by no means certain <sup>3</sup>. </p>-<p>An association with <a title="NF1" href="/articles/nf1">neurofibromatosis type I (NF1)</a> has been reported <sup>3-4</sup>. </p>-<h4>Clinical presentation</h4>-<p>Their expansion within the <a href="/articles/brainstem">brainstem</a> causes narrowing the <a href="/articles/aqueduct-of-sylvius">aqueduct of Sylvius</a> and causing <a href="/articles/obstructive_hydrocephalus">obstructive hydrocephalus</a> with presentation usually secondary to headache <sup>3-4</sup>. </p>-<p>Additional symptoms may include gaze palsies, due to compression of the <a href="/articles/medial-longitudinal-fasiculus">medial longitudinal fasiculus</a> leading to an upgaze pasly, diplopia or <a href="/articles/parinaud-syndrome">Parinaud syndrome</a>, although these are uncommon <sup>3-4</sup>. </p>-<h4>Pathology</h4>-<p>The vast majority of lesions are low grade astrocytoma, although occasionally other glial series tumours are encountered in the tectal region including <a title="Ependymoma" href="/articles/ependymoma">ependymoma</a>, <a title="Ganglioglioma" href="/articles/ganglioglioma">ganglioglioma</a> and <a title="CNS primitive neuroectodermal tumour (PNET)" href="/articles/primitive-neuroectodermal-tumour-of-the-cns">primitive neuroectodermal tumours (PNET) </a><sup>3</sup>. </p>-<h4>Radiographic features</h4>-<h6>CT</h6>-<p>Typical CT finding is homogenous expansion of tectal plate, isodense to grey matter with minimal enhancement in postcontrast images <sup>1,3</sup>. </p>-<p>On CT it is not uncommon to find a central tectal calcification <sup>2-3</sup>.</p>-<h5>MRI</h5>-<p>Typically the tumours demonstrate expansion of the tectal plate by a solid nodule of tisse. </p>-<ul>- +<p><strong>Tectal gliomas</strong> fall under the grouping of childhood <a href="/articles/brainstem-glioma">brainstem gliomas</a> and unlike the other tumours in that group they are typically low grade <a href="/articles/astrocytic-tumours">astrocytomas</a> with good prognosis. </p><h4>Epidemiology</h4><p>Tectal plate gliomas are encountered in children and adolescents <sup>4</sup>. A male predilection has sometimes been reported although this is by no means certain <sup>3</sup>. </p><p>An association with <a href="/articles/nf1">neurofibromatosis type I (NF1)</a> has been reported <sup>3-4</sup>. </p><h4>Clinical presentation</h4><p>Their expansion within the <a href="/articles/brainstem">brainstem</a> causes narrowing the <a href="/articles/aqueduct-of-sylvius">aqueduct of Sylvius</a> and causing <a href="/articles/obstructive-hydrocephalus">obstructive hydrocephalus</a> with presentation usually secondary to headache <sup>3-4</sup>. </p><p>Additional symptoms may include gaze palsies, due to compression of the <a href="/articles/medial-longitudinal-fasiculus">medial longitudinal fasciculus</a> leading to an upgaze palsy, diplopia or <a href="/articles/parinaud-syndrome">Parinaud syndrome</a>, although these are uncommon <sup>3-4</sup>. </p><h4>Pathology</h4><p>The vast majority of lesions are low grade astrocytoma, although occasionally other glial series tumours are encountered in the tectal region including <a href="/articles/ependymoma">ependymoma</a>, <a href="/articles/ganglioglioma">ganglioglioma</a> and <a href="/articles/primitive-neuroectodermal-tumour-of-the-cns">primitive neuroectodermal tumours (PNET) </a><sup>3</sup>. </p><h4>Radiographic features</h4><h6>CT</h6><p>Typical CT finding is homogeneous expansion of tectal plate, isodense to grey matter with minimal enhancement on postcontrast images <sup>1,3</sup>. On CT it is not uncommon to find a central tectal calcification <sup>2-3</sup>.</p><h5>MRI</h5><p>Typically the tumours demonstrate expansion of the tectal plate by a solid nodule of tissue. </p><ul>
-<strong>T1</strong> - iso to slightly hypointense to grey matter <sup>1-3</sup>-</li>- +<strong>T1:</strong> iso to slightly hypointense to grey matter <sup>1-3</sup>
- +</li>
-<strong>T2</strong> - hyperintense to grey matter </li>- +<strong>T2:</strong> hyperintense to grey matter </li>
-<strong>T1 C+ (Gd)</strong> : usually no enhancement </li>-</ul><p>With time the mass can develop small cystic spaces (sometimes associated with neurological deficits) or calcification <sup>3</sup>. </p>-<p>Higher grade tumours tend to be larger and tend to enhance more vividly <sup>3</sup>. </p>-<h4>Treatment and prognosis</h4>-<p>As tectal plate gliomas are low grade and often very slow growing, shunting is often the only required intervention for long term survival. As surgical biopsy can have significant morbidity in this area, usually the diagnosis is made on imaging findings alone. </p>-<p>In the minority of patients who progress, radiotherapy often leads to local control or even tumour regression <sup>2</sup>. Surgical excision is sometimes necessary <sup>3</sup>. </p>-<p>Imaging predictors of patients who will need further treatment include a size greater than 2.5cm and presence of contrast enhancement <sup>3</sup>. </p>-<h4>Differential diagnosis</h4>-<p>When the tectum is near-normal then the differential is largely limited to:</p>-<ul><li>-<a title="Aqueductal stenosis" href="/articles/aqueduct_stenosis">aqueductal stenosis</a>-<ul>-<li>no mass lesion</li>- +<strong>T1 C+ (Gd):</strong> usually no enhancement </li>
- +</ul><p>With time the mass can develop small cystic spaces (sometimes associated with neurological deficits) or calcification <sup>3</sup>. </p><p>Higher grade tumours tend to be larger and tend to enhance more vividly <sup>3</sup>. </p><h4>Treatment and prognosis</h4><p>As tectal plate gliomas are low grade and often very slow growing, shunting is often the only required intervention for long term survival. As surgical biopsy can have significant morbidity in this area, usually the diagnosis is made on imaging findings alone. </p><p>In the minority of patients who progress, radiotherapy often leads to local control or even tumour regression <sup>2</sup>. Surgical excision is sometimes necessary <sup>3</sup>. </p><p>Imaging predictors of patients who will need further treatment include a size greater than 2.5 cm and presence of contrast enhancement <sup>3</sup>. </p><h4>Differential diagnosis</h4><p>When the tectum is near-normal then the differential is largely limited to:</p><ul><li>
- +<a href="/articles/aqueduct-stenosis">aqueductal stenosis</a><ul>
- +<li>no mass lesion</li>
-</li></ul><p>With larger lesions, where the mass is not definitely arising from the tectal plate then the differential is essentially that of a pineal region mass and therefore includes: </p>-<ul>- +</li></ul><p>With larger lesions, where the mass is not definitely arising from the tectal plate then the differential is essentially that of a pineal region mass and therefore includes: </p><ul>
-<a title="Pineal parenchymal tumours" href="/articles/pineal-parenchymal-tumours">pineal parenchymal tumours</a> and <a title="Intracranial germ cell tumours" href="/articles/intracranial-germ-cell-tumours">germ cell tumours</a> </li>-<li><a title="Pineal cyst" href="/articles/pineal_cyst">pineal cyst</a></li>-<li><a title="Meningioma" href="/articles/meningioma">meningioma</a></li>- +<a href="/articles/pineal-parenchymal-tumours">pineal parenchymal tumours</a> and <a href="/articles/intracranial-germ-cell-tumours">germ cell tumours</a>
- +</li>
- +<li><a href="/articles/pineal-cyst">pineal cyst</a></li>
- +<li><a href="/articles/meningioma">meningioma</a></li>
-<a title="Cerebral metastasis" href="/articles/cerebral-metastases">cerebral metastasis</a> </li>-<li><a title="Cavernous malformation" href="/articles/cavernous-haemangiomas">cavernous malformation</a></li>-</ul><p>In patients with <a title="NF1" href="/articles/neurofibromatosis-type-1">NF1</a> a hamartoma should also be considered. They tend to have some T1 hyperintensity <sup>4</sup>. </p>- +<a href="/articles/cerebral-metastases">cerebral metastasis</a> </li>
- +<li><a href="/articles/cavernous-venous-malformation-1">cavernous malformation</a></li>
- +</ul><p>In patients with <a href="/articles/neurofibromatosis-type-1">NF1</a> a hamartoma should also be considered. They tend to have some T1 hyperintensity <sup>4</sup>. </p>
Image 8 MRI (T1 C+) ( update )
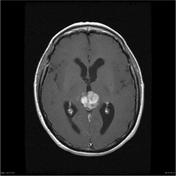
Image 9 CT (non-contrast) ( create )








 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.