Peroneus brevis tear
Updates to Article Attributes
Introduction
CLINICAL INFO:Peroneus brevis tendon tears
- Man can present with lateral ankle pain with or without a history of trauma, 46 years oldworsening with activity. These can typically be managed conservatively with ultrasound or MRI useful in the diagnosis.
Epidemiology
- PainLittle epidemiological information available but patients typically are younger and active, with an athletic background.
Clinical presentation
Symptoms can include pain, swelling and erythema at the external malleolus for several weekslateral ankle which worsens with activity, or may be asymptomatic. Some tears occur following trauma, although there is a degenerative process which does not require an isolated episode. There is a suspected high rate of peroneal tendon injury in those with chronic ankle instability. There is also an association with systemic conditions e.g. rheumatoid arthritis, diabetes, or local steroid injection 1.
Pathology
ULTRASOUND:
Longitudinal split tear ofAs the peroneus brevis tendon sits between the peroneus longus tendon and the bony retromalleolar groove of the fibula it is at risk of degenerative tear, particularly in dorsiflexion.
Traumatic episodes and tendon dislocation can lead to degeneration. Other anatomical variants can predispose to injury:
- insufficiency of the overlying superior peroneal retinaculum
- low lying peroneus brevis muscle belly or variant peroneus quartus muscle
As the brevis tear develops, the longus tendon moves forward into the space which further antagonises the injury and prevents healing.
One surgical review stated 40% of those undergoing brevis repair had longus tears at surgery 2 which are likely secondary to degenerative change following migration.
Radiographic features
Ultrasound
Ultrasound has a high sensitivity (100%) and specificity (85%) for identifying tendon tears 3.
-
partial tear: discontinuity and partial retraction of affected tendon fibres with
'boomerangfluid in the sheath, normal appearance proximal and distal to the tear - longitudinal fissures: two "hemi-tendon" appearance at the apex of the malleolus affecting the deep fibres first
- full thickness: typical appearance of rupture
MRI
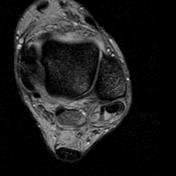
Torn peroneus brevis tendons have a characteristic C-shape or "boomerang" appearance, with the tendon enveloping the peroneus longus tendon. Other signs include distortion of the tendon, increased T1w and T2w signal, with anterior migration of the peroneus longus tendon.
Treatment and prognosis
Typically managed conservatively with anti-inflammatories and rest/immobilisation. Surgical fixation can be considered in persisting cases or for those with ankle instability with debridement or if required tenodesis to the adjacent peroneus longus tendon.
Differential diagnosis
- normal variant bifurcated peroneus brevis tendon: differentiate by identifying muscle fibres attaching to the tendon slips
- peroneus quartus tendon insertion simulating a tear on imaging
See also
-<p><strong>CLINICAL INFO:</strong></p><p>- Man, 46 years old.</p><p>- Pain at the external malleolus for several weeks.</p><p> </p><p><strong>ULTRASOUND:</strong></p><p>Longitudinal split tear of the peroneus brevis tendon with 'boomerang sign' on ultrasound.</p>- +<h4>Introduction</h4><p><strong>Peroneus brevis tendon tears</strong> can present with lateral ankle pain with or without a history of trauma, worsening with activity. These can typically be managed conservatively with ultrasound or MRI useful in the diagnosis.</p><h4>Epidemiology</h4><p>Little epidemiological information available but patients typically are younger and active, with an athletic background.</p><h4>Clinical presentation</h4><p>Symptoms can include pain, swelling and erythema at the lateral ankle which worsens with activity, or may be asymptomatic. Some tears occur following trauma, although there is a degenerative process which does not require an isolated episode. There is a suspected high rate of peroneal tendon injury in those with chronic ankle instability. There is also an association with systemic conditions e.g. rheumatoid arthritis, diabetes, or local steroid injection <sup>1</sup>.</p><h4>Pathology</h4><p>As the peroneus brevis tendon sits between the peroneus longus tendon and the bony retromalleolar groove of the fibula it is at risk of degenerative tear, particularly in dorsiflexion.</p><p>Traumatic episodes and tendon dislocation can lead to degeneration. Other anatomical variants can predispose to injury:</p><ul>
- +<li>insufficiency of the overlying superior peroneal retinaculum</li>
- +<li>low lying peroneus brevis muscle belly or variant peroneus quartus muscle</li>
- +</ul><p>As the brevis tear develops, the longus tendon moves forward into the space which further antagonises the injury and prevents healing.</p><p>One surgical review stated 40% of those undergoing brevis repair had longus tears at surgery <sup>2 </sup>which are likely secondary to degenerative change following migration.</p><h4>Radiographic features</h4><h5>Ultrasound</h5><p>Ultrasound has a high sensitivity (100%) and specificity (85%) for identifying tendon tears <sup>3</sup>.</p><ul>
- +<li>partial tear: discontinuity and partial retraction of affected tendon fibres with fluid in the sheath, normal appearance proximal and distal to the tear</li>
- +<li>longitudinal fissures: two "hemi-tendon" appearance at the apex of the malleolus affecting the deep fibres first</li>
- +<li>full thickness: typical appearance of rupture</li>
- +</ul><h5>MRI</h5><p>Torn peroneus brevis tendons have a characteristic C-shape or "boomerang" appearance, with the tendon enveloping the peroneus longus tendon. Other signs include distortion of the tendon, increased T1w and T2w signal, with anterior migration of the peroneus longus tendon.</p><h4>Treatment and prognosis</h4><p>Typically managed conservatively with anti-inflammatories and rest/immobilisation. Surgical fixation can be considered in persisting cases or for those with ankle instability with debridement or if required tenodesis to the adjacent peroneus longus tendon.</p><h4>Differential diagnosis</h4><ul>
- +<li>normal variant bifurcated peroneus brevis tendon: differentiate by identifying muscle fibres attaching to the tendon slips</li>
- +<li>peroneus quartus tendon insertion simulating a tear on imaging</li>
- +</ul><h4>See also</h4><ul>
- +<li><a href="/articles/peroneus-brevis-muscle">Peroneus brevis muscle</a></li>
- +<li><a href="/articles/boomerang-sign-1">Boomerang sign</a></li>
- +</ul>
References changed:
- 1. Wang XT, Rosenberg ZS, Mechlin MB, Schweitzer ME. Normal variants and diseases of the peroneal tendons and superior peroneal retinaculum: MR imaging features. Radiographics : a review publication of the Radiological Society of North America, Inc. 25 (3): 587-602. <a href="https://doi.org/10.1148/rg.253045123">doi:10.1148/rg.253045123</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/15888611">Pubmed</a> <span class="ref_v4"></span>
- 1. Wang XT, Rosenberg ZS, Mechlin MB, Schweitzer ME. Normal variants and diseases of the peroneal tendons and superior peroneal retinaculum: MR imaging features. Radiographics : a review publication of the Radiological Society of North America, Inc. 25 (3): 587-602. <a href="https://doi.org/10.1148/rg.253045123">doi:10.1148/rg.253045123</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/15888611">Pubmed</a> <span class="ref_v4"></span>
- 2. Dombek MF, Lamm BM, Saltrick K, Mendicino RW, Catanzariti AR. Peroneal tendon tears: a retrospective review. The Journal of Foot and Ankle Surgery. 42 (5): 250-258. <a href="https://doi.org/doi:10.1016/S1067-2516(03)00314-4">doi:doi:10.1016/S1067-2516(03)00314-4</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/14566716">Pubmed</a> <span class="ref_v4"></span>
- 3. Molini L, Bianchi S. US in peroneal tendon tear. Journal of ultrasound. 17 (2): 125-34. <a href="https://doi.org/10.1007/s40477-014-0072-y">doi:10.1007/s40477-014-0072-y</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/24883136">Pubmed</a> <span class="ref_v4"></span>
- Dombek MF, Lamm BM, Saltrick K, Mendicino RW, Catanzariti AR. Peroneal tendon tears: a retrospective review. The Journal of Foot and Ankle Surgery. 42 (5): 250-258. <a href="https://doi.org/doi:10.1016/S1067-2516(03)00314-4">doi:doi:10.1016/S1067-2516(03)00314-4</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/14566716">Pubmed</a> <span class="ref_v4"></span>
Image 1 Ultrasound (Transverse) ( create )

Image 2 MRI (T2*) ( create )







 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.