Pleomorphic xanthoastrocytoma
Updates to Article Attributes
Pleomorphic xanthoastrocytomas xanthoastrocytomas (PXA) are a type of rare, low-grade astrocytoma (WHO Grade II) found in young patients who typically present with temporal lobe epilepsy.
They usually present as cortical tumours with a cystic component and vivid contrast enhancement. Features of slow growth may be present, such as no surrounding oedema and scalloping of the overlying bone. A reactive dural involvement expressed by a dural tail sign can be found. Calcifications are rare.
Epidemiology
They are rare tumours accounting for only ~ 1% of primary brain tumours2-3.
Clinical presentation
Typically these tumours are found in young patients (children or young adults), and as they have a predilection for the temporal lobe, they most frequently present with seizures (~ 75% of cases ) 1,2. Other findings include dizziness, and headache or rarely patients are asymptomatic 5.
Pathology
Macroscopically these tumours appear well circumscribed, often with cystic component and involvement of the overlying leptomeninges 1,3.
Microscopically the margins are not as well defined. Spindle cells, polygonal cells, multi-nucleated cells and lipid laden xanthomatous astrocytes are identified. Even more pleomorphic is the appearance of the nuclei. Endothelial proliferation is rare.
Markers
These tumours are GFAP positive, although often only weakly 3.
Location
PXAs are almost invariably (98%) located supratentorially, typically located superficially (peripherally) abutting the leptomeninges, involving the cortex and overlying leptomeninges but dural involvement is rare. Approximately half are located in the temporal lobe with rest of lesions are more common in frontal and then parietal lobes 24.
Radiographic features
Often there is a cystic component (50-60%) with an enhancing mural nodule or only solid nodule. Additionally, they are one of the tumours that may exhibit a dural tail, which is reactive rather than due to direct dural invasion, which is rare 2. As these lesions are very slow growing and superficial remodelling of the adjacent skull is characteristics and vasogenic oedema is variable 5.
CT
PXAs are typically hypo or isodense and may be well or poorly demarcated, usually with no or little surrounding oedema. Calcification is rare. Due to its superficalsuperficial location it may cause scalloping of the overlying bone 2.
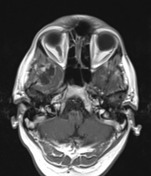
MRI
-
T1
- solid component iso to hypointense c.f. grey matter
- cystic component low signal
- leptomeningeal involvement seen in over 70% of cases 2
-
T1 C+
(Gd)- solid component usually enhances vividly
-
T2
- solid component iso to hyperintense c.f. grey matter
- cystic component high signal
- on T2 FLAIR sequence, cystic areas show hyperintensity relative to CSF due to higher protein contents
- little surrounding vasogenic oedema
DSA - angiography
Despite vivid enhancement, PXAs are usually avascular on angiography 2
Treatment and prognosis
Although prognosis is good following surgical excision, with a 5 year-year survival of 70 -80% 1,3, local recurrence and malignant transformation (to WHO grade III lesion or GBM) are not uncommon (up to 20% cases) 2.
Neither radiotherapy nor chemotherapy havehas a significant effect on these tumours 2, although radiotherapy may have a role to play in patients with incomplete resection or those with recurrent disease 3.
Differential diagnosis
Main differential diagnosis is that of other cortical tumours, with helpful distinguishing features including1-4:
-
ganglioglioma
- can look very similar
- contrast enhancement often less prominent
- calcification in ~50% of cases
- no dural tail
signsign
-
dysembryoplastic neuroepithelial tumours (DNET)
- contrast enhancement uncommon
- 'bubbly appearance' common
-
oligodendroglioma
- calcifications common
-
desmoplastic infantile ganglioglioma
- young children
- dural involvement prominent
- large often multiple lesions
See also
-<p><strong>Pleomorphic xanthoastrocytomas (PXA)</strong> are a type of rare, low-grade <a href="/articles/astrocytic-tumours">astrocytoma</a> (<a href="/articles/cns-tumours-classification-and-grading-who">WHO Grade II</a>) found in young patients who typically present with <a href="/articles/temporal-lobe-epilepsy">temporal lobe epilepsy</a>.</p><p>They usually present as cortical tumours with a cystic component and vivid contrast enhancement. Features of slow growth may be present, such as no surrounding oedema and scalloping of the overlying bone. A reactive dural involvement expressed by a dural tail sign can be found. Calcifications are rare. </p><h4>Epidemiology</h4><p>They are rare tumours accounting for only ~ 1% of primary<a href="/articles/brain-tumours"> brain tumours </a><sup>2-3</sup>. </p><h4>Clinical presentation</h4><p>Typically these tumours are found in young patients (children or young adults), and as they have a predilection for the temporal lobe, they most frequently present with seizures (~ 75% of cases ) <sup>1,2</sup>.</p><h4>Pathology</h4><p>Macroscopically these tumours appear well circumscribed, often with cystic component and involvement of the overlying <a href="/articles/leptomeninges">leptomeninges</a> <sup>1,3</sup>.</p><p>Microscopically the margins are not as well defined. Spindle cells, polygonal cells, multi-nucleated cells and lipid laden xanthomatous astrocytes are identified. Even more pleomorphic is the appearance of the nuclei. Endothelial proliferation is rare. </p><h5>Markers</h5><p>These tumours are <a href="/articles/gfap">GFAP</a> positive, although often only weakly <sup>3</sup>.</p><h5>Location</h5><p>PXAs are almost invariably (98%) located supratentorially, typically located superficially (peripherally), involving the cortex and overlying leptomeninges. Approximately half are located in the temporal lobe <sup>2</sup>.</p><h4>Radiographic features</h4><p>Often there is a cystic component (50-60%) with an enhancing mural nodule. Additionally they are one of the tumours that may exhibit a <a href="/articles/dural-tail-sign-1">dural tail</a>, which is reactive rather than due to direct dural invasion, which is rare <sup>2</sup>. </p><h5>CT</h5><p>PXAs are typically hypo or isodense and may be well or poorly demarcated, usually with little surrounding oedema. Calcification is rare. Due to its superfical location it may cause scalloping of the overlying bone <sup>2</sup>.</p><h5>MRI</h5><ul>- +<p><strong>Pleomorphic xanthoastrocytomas (PXA)</strong> are a type of rare, low-grade <a href="/articles/astrocytic-tumours">astrocytoma</a> (<a href="/articles/cns-tumours-classification-and-grading-who">WHO Grade II</a>) found in young patients who typically present with <a href="/articles/temporal-lobe-epilepsy">temporal lobe epilepsy</a>.</p><p>They usually present as cortical tumours with a cystic component and vivid contrast enhancement. Features of slow growth may be present, such as no surrounding oedema and scalloping of the overlying bone. A reactive dural involvement expressed by a dural tail sign can be found. Calcifications are rare. </p><h4>Epidemiology</h4><p>They are rare tumours accounting for only ~ 1% of primary<a href="/articles/brain-tumours"> brain tumours </a><sup>2-3</sup>. </p><h4>Clinical presentation</h4><p>Typically these tumours are found in young patients (children or young adults), and as they have a predilection for the temporal lobe, they most frequently present with seizures (~ 75% of cases ) <sup>1,2</sup>. Other findings include dizziness, and headache or rarely patients are asymptomatic <sup> 5</sup>.</p><h4>Pathology</h4><p>Macroscopically these tumours appear well circumscribed, often with cystic component and involvement of the overlying <a href="/articles/leptomeninges">leptomeninges</a> <sup>1,3</sup>.</p><p>Microscopically the margins are not as well defined. Spindle cells, polygonal cells, multi-nucleated cells and lipid laden xanthomatous astrocytes are identified. Even more pleomorphic is the appearance of the nuclei. Endothelial proliferation is rare. </p><h5>Markers</h5><p>These tumours are <a href="/articles/gfap">GFAP</a> positive, although often only weakly <sup>3</sup>.</p><h5>Location</h5><p>PXAs are almost invariably (98%) located supratentorially, typically located superficially (peripherally) abutting the leptomeninges, involving the cortex and overlying leptomeninges but dural involvement is rare. Approximately half are located in the temporal lobe with rest of lesions are more common in frontal and then parietal lobes <sup>4</sup>.</p><h4>Radiographic features</h4><p>Often there is a cystic component (50-60%) with an enhancing mural nodule or only solid nodule. Additionally, they are one of the tumours that may exhibit a <a href="/articles/dural-tail-sign-1">dural tail</a>, which is reactive rather than due to direct dural invasion, which is rare <sup>2</sup>. As these lesions are very slow growing and superficial remodelling of the adjacent skull is characteristics and vasogenic oedema is variable <sup>5</sup>. </p><h5>CT</h5><p>PXAs are typically hypo or isodense and may be well or poorly demarcated, usually with no or little surrounding oedema. Calcification is rare. Due to its superficial location it may cause scalloping of the overlying bone <sup>2</sup>.</p><h5>MRI</h5><ul>
-<strong>T1 C+</strong><strong> (Gd)</strong><ul><li>solid component usually enhances vividly</li></ul>- +<strong>T1 C+</strong><strong> (Gd)</strong><ul><li>solid component usually enhances vividly</li></ul>
- +<li>on T2 FLAIR sequence, cystic areas show hyperintensity relative to CSF due to higher protein contents</li>
-</ul><h5>DSA - angiography</h5><p>Despite vivid enhancement, PXAs are usually avascular on angiography <sup>2</sup></p><h4>Treatment and prognosis</h4><p>Although prognosis is good following surgical excision, with a 5 year survival of 70 -80% <sup>1,3</sup>, local recurrence and malignant transformation (to WHO grade III lesion or GBM) are not uncommon (up to 20% cases) <sup>2</sup></p><p>Neither radiotherapy nor chemotherapy have a significant effect on these tumours <sup>2</sup>, although radiotherapy may have a role to play in patients with incomplete resection or those with recurrent disease <sup>3</sup>. </p><h4>Differential diagnosis</h4><p>Main differential diagnosis is that of other cortical tumours, with helpful distinguishing features including <sup>1-4</sup>: </p><ul>- +</ul><h5>DSA - angiography</h5><p>Despite vivid enhancement, PXAs are usually avascular on angiography <sup>2</sup></p><h4>Treatment and prognosis</h4><p>Although prognosis is good following surgical excision, with a 5-year survival of 70 -80% <sup>1,3</sup>, local recurrence and malignant transformation (to WHO grade III lesion or GBM) are not uncommon (up to 20% cases) <sup>2</sup>.</p><p>Neither radiotherapy nor chemotherapy has a significant effect on these tumours <sup>2</sup>, although radiotherapy may have a role to play in patients with incomplete resection or those with recurrent disease <sup>3</sup>. </p><h4>Differential diagnosis</h4><p>Main differential diagnosis is that of other cortical tumours, with helpful distinguishing features including <sup>1-4</sup>: </p><ul>
-<li>no <a href="/articles/dural-tail-sign-1">dural tail sign</a>- +<li>no <a href="/articles/dural-tail-sign-1">dural tail sign</a>
-<a href="/articles/dysembryoplastic-neuroepithelial-tumour">dysembryoplastic neuroepithelial tumours (DNET)</a><ul>- +<a href="/articles/dysembryoplastic-neuroepithelial-tumour">dysembryoplastic neuroepithelial tumours (DNET) </a><ul>
References changed:
- 1. Koeller K & Rushing E. From the Archives of the AFIP: Pilocytic Astrocytoma: Radiologic-Pathologic Correlation. Radiographics. 2004;24(6):1693-708. <a href="https://doi.org/10.1148/rg.246045146">doi:10.1148/rg.246045146</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/15537977">Pubmed</a>
- 2. Zoran Rumboldt, Mauricio Castillo, Benjamin Huang et al. Brain Imaging with MRI and CT. (2012) ISBN: 9781139576390 - <a href="http://books.google.com/books?vid=ISBN9781139576390">Google Books</a>
- 3. Rippe D, Boyko O, Radi M, Worth R, Fuller G. MRI of Temporal Lobe Pleomorphic Xanthoastrocytoma. J Comput Assist Tomogr. 1992;16(6):856-9. <a href="https://doi.org/10.1097/00004728-199211000-00004">doi:10.1097/00004728-199211000-00004</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/1385498">Pubmed</a>
- 4. Crespo-Rodríguez A, Smirniotopoulos J, Rushing E. MR and CT Imaging of 24 Pleomorphic Xanthoastrocytomas (PXA) and a Review of the Literature. Neuroradiology. 2007;49(4):307-15. <a href="https://doi.org/10.1007/s00234-006-0191-z">doi:10.1007/s00234-006-0191-z</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/17205313">Pubmed</a>
- 5. Yu S, He L, Zhuang X, Luo B. Pleomorphic Xanthoastrocytoma: MR Imaging Findings in 19 Patients. Acta Radiol. 2011;52(2):223-8. <a href="https://doi.org/10.1258/ar.2010.100221">doi:10.1258/ar.2010.100221</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/21498352">Pubmed</a>
- 1. Kaye AH, Laws ER. Brain tumors, an encyclopedic approach. Gulf Professional Publishing. (2001) ISBN:0443064261. <a href="http://books.google.com/books?vid=ISBN0443064261">Read it at Google Books</a> - <a href="http://www.amazon.com/gp/product/0443064261?ie=UTF8&tag=radiopaediaor-20&linkCode=as2&camp=1789&creative=9325&creativeASIN=0443064261">Find it at Amazon</a><div class="ref_v2"></div>
- 2. Koeller KK, Rushing EJ. From the archives of the AFIP: pilocytic astrocytoma: radiologic-pathologic correlation. Radiographics. 24 (6): 1693-708. <a href="http://dx.doi.org/10.1148/rg.246045146">doi:10.1148/rg.246045146</a> - <a href="http://www.ncbi.nlm.nih.gov/pubmed/15537977">Pubmed citation</a><div class="ref_v2"></div>
- 3. Rolf J, Fairfax K, Turner M. Signaling pathways in T follicular helper cells. J. Immunol. 2010;184 (12): 6563-8. <a href="http://dx.doi.org/10.4049/jimmunol.1000202">doi:10.4049/jimmunol.1000202</a> - <a href="http://www.ncbi.nlm.nih.gov/pubmed/20525897">Pubmed citation</a><div class="ref_v2"></div>
- 4. Rumboldt Z, Castillo M, Huang B et-al. Brain Imaging with MRI and CT. Cambridge University Press. (2012) ISBN:1139576399. <a href="http://books.google.com/books?vid=ISBN1139576399">Read it at Google Books</a> - <a href="http://www.amazon.com/gp/product/1139576399">Find it at Amazon</a><span class="auto"></span>
Image 7 MRI (T1 C+) ( create )







 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.