Reverse total shoulder arthroplasty
- Integral Diagnostics, Shareholder (ongoing)
- Micro-X Ltd, Shareholder (ongoing)
Updates to Article Attributes
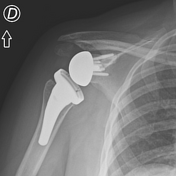
A reverse total shoulder arthroplasty (RTSA) or replacement (RTSR) is a variant on the standard total shoulder replacement (TSR). It is often the preferred method when there has been advanced damage to the rotator cuff as seen in rotator cuff arthropathy.
Procedure
The reverse total shoulder arthroplasty flips the normal mechanical arrangement of the shoulder's ball-and-socket joint. Instead of the humeral head fitting into the glenoid, a rounded hemispheric glenoid prosthesis articulates with a socket on the humeral head prosthesis.
Advantages and disadvantages
Reversing the ball and socket arrangement, the point of rotation is moved more medially, aiding the deltoid muscle which, without an intact rotator cuff, will provide most of the early adduction for the upper extremity after the surgery. Internal and external rotation are more limited in this arrangement, however.
The indications for reverse total shoulder replacement are expanding and include
osteoarthritis in patients with a degenerate rotator cuff
irreparable massive cuff tear
replacement after tumour surgery
complex fractures in elderly patients where the greater and lesser tuberosity fragments are involved
failed standard total shoulder replacement
Axillary nerve dysfunction is a contraindication for reverse total shoulder replacement.
The design is thought to have relatively good short and medium-term outcomes compared with other types of total shoulder replacements, with improved recovery time and pain scores 3. Long-term outcomes remain poorly defined.
Radiographic features
Plain radiograph
neutral AP view (Grashey view) and axillary views obtained
>2 mm of lucency around the prosthetic component is concerning for loosening
"scapular notching" (erosion of the inferior scapular neck) is suggestive of glenoid component failure
periprosthetic fractures at the base of the acromion at the scapular spine are more common
CT
better for evaluation if there is a suboptimal radiograph
as on conventional radiography, >2 mm of lucency around the prosthetic component is concerning for loosening
MRI
metal artifact reduction techniques have improved the ability to image prostheses on MRI
Ultrasound
useful for imaging the rotator cuff musculature, evaluating the prosthesis dynamically, and evaluating for joint effusion
cannot be used to evaluate for component loosening
Complications
The overall complication rate for all forms of total shoulder arthroplasty is ~15%. Complications include:
aseptic loosening of the glenoid component: most common complication (~30% of all shoulder replacements, but decreased with reverse total shoulder replacements 5)
aseptic loosening of the humeral component
dislocation
periprosthetic fractures
acromial/scapular spine fracture, most commonly a stress fracture 6
hardware failure
axillary nerve palsy
infection (uncommon)
acromionstress fracture
-<p>A<strong> reverse total shoulder arthroplasty (RTSA) </strong>or <strong>replacement</strong> (<strong>RTSR</strong>) is a variant on the <a href="/articles/total-shoulder-arthroplasty-1">standard total shoulder replacement (TSR)</a>. It is often the preferred method when there has been advanced damage to the <a href="/articles/rotator-cuff">rotator cuff</a> as seen in <a href="/articles/rotator-cuff-tear-arthropathy">rotator cuff arthropathy</a>.</p><h4>Procedure</h4><p>The reverse total shoulder arthroplasty flips the normal mechanical arrangement of the shoulder's ball-and-socket joint. Instead of the humeral head fitting into the glenoid, a rounded hemispheric glenoid prosthesis articulates with a socket on the humeral head prosthesis.</p><h4>Advantages and disadvantages</h4><p>Reversing the ball and socket arrangement, the point of rotation is moved more medially, aiding the <a href="/articles/deltoid-muscle">deltoid muscle</a> which, without an intact rotator cuff, will provide most of the early adduction for the upper extremity after the surgery. Internal and external rotation are more limited in this arrangement, however.</p><p>The indications for reverse total shoulder replacement are expanding and include</p><ul>-<li><p><a href="/articles/osteoarthritis">osteoarthritis</a> in patients with a degenerate rotator cuff</p></li>-<li><p>irreparable <a href="/articles/full-thickness-rotator-cuff-tear-1">massive cuff tear</a></p></li>-<li><p>replacement after tumour surgery</p></li>-<li><p>complex fractures in elderly patients where the greater and lesser tuberosity fragments are involved </p></li>-<li><p>failed standard total shoulder replacement</p></li>-</ul><p><a href="/articles/axillary-nerve-dysfunction">Axillary nerve dysfunction</a> is a contraindication for reverse total shoulder replacement. </p><p>The design is thought to have relatively good short and medium-term outcomes compared with other types of total shoulder replacements, with improved recovery time and pain scores <sup>3</sup>. Long-term outcomes remain poorly defined.</p><h4>Radiographic features</h4><h5>Plain radiograph</h5><ul>-<li><p>neutral AP view (<a href="/articles/shoulder-ap-glenoid-view">Grashey view</a>) and <a href="/articles/axillary-views">axillary views</a> obtained</p></li>-<li><p>>2 mm of lucency around the prosthetic component is concerning for loosening</p></li>-<li><p><a href="/articles/scapular-notching">"scapular notching"</a> (erosion of the inferior scapular neck) is suggestive of glenoid component failure</p></li>-<li><p><a href="/articles/periprosthetic-fracture">periprosthetic fractures</a> at the base of the acromion at the scapular spine are more common</p></li>-</ul><h5>CT</h5><ul>-<li><p>better for evaluation if there is a suboptimal radiograph</p></li>-<li><p>as on conventional radiography, >2 mm of lucency around the prosthetic component is concerning for loosening</p></li>-</ul><h5>MRI</h5><ul><li><p><a href="/articles/metal-artifact-reduction-sequence">metal artifact reduction techniques</a> have improved the ability to image prostheses on MRI</p></li></ul><h5>Ultrasound</h5><ul>-<li><p>useful for imaging the rotator cuff musculature, evaluating the prosthesis dynamically, and evaluating for joint effusion</p></li>-<li><p>cannot be used to evaluate for component loosening</p></li>-</ul><h4>Complications</h4><p>The overall complication rate for all forms of total shoulder arthroplasty is ~15%. Complications include:</p><ul>-<li><p>aseptic loosening of the glenoid component: most common complication (~30% of all shoulder replacements, but decreased with reverse total shoulder replacements <sup>5</sup>)</p></li>-<li><p>aseptic loosening of the humeral component</p></li>-<li><p>dislocation</p></li>-<li><p>periprosthetic fractures</p></li>-<li><p>hardware failure</p></li>-<li><p>axillary nerve palsy</p></li>-<li><p>infection (uncommon)</p></li>-<li><p>acromion <a href="/articles/stress-fracture-2">stress fracture</a></p></li>- +<p>A<strong> reverse total shoulder arthroplasty (RTSA) </strong>or <strong>replacement</strong> (<strong>RTSR</strong>) is a variant on the <a href="/articles/total-shoulder-arthroplasty-1">standard total shoulder replacement (TSR)</a>. It is often the preferred method when there has been advanced damage to the <a href="/articles/rotator-cuff">rotator cuff</a> as seen in <a href="/articles/rotator-cuff-tear-arthropathy">rotator cuff arthropathy</a>.</p><h4>Procedure</h4><p>The reverse total shoulder arthroplasty flips the normal mechanical arrangement of the shoulder's ball-and-socket joint. Instead of the humeral head fitting into the glenoid, a rounded hemispheric glenoid prosthesis articulates with a socket on the humeral head prosthesis.</p><h4>Advantages and disadvantages</h4><p>Reversing the ball and socket arrangement, the point of rotation is moved more medially, aiding the <a href="/articles/deltoid-muscle">deltoid muscle</a> which, without an intact rotator cuff, will provide most of the early adduction for the upper extremity after the surgery. Internal and external rotation are more limited in this arrangement, however.</p><p>The indications for reverse total shoulder replacement are expanding and include</p><ul>
- +<li><p><a href="/articles/osteoarthritis">osteoarthritis</a> in patients with a degenerate rotator cuff</p></li>
- +<li><p>irreparable <a href="/articles/full-thickness-rotator-cuff-tear-1">massive cuff tear</a></p></li>
- +<li><p>replacement after tumour surgery</p></li>
- +<li><p>complex fractures in elderly patients where the greater and lesser tuberosity fragments are involved </p></li>
- +<li><p>failed standard total shoulder replacement</p></li>
- +</ul><p><a href="/articles/axillary-nerve-dysfunction">Axillary nerve dysfunction</a> is a contraindication for reverse total shoulder replacement. </p><p>The design is thought to have relatively good short and medium-term outcomes compared with other types of total shoulder replacements, with improved recovery time and pain scores <sup>3</sup>. Long-term outcomes remain poorly defined.</p><h4>Radiographic features</h4><h5>Plain radiograph</h5><ul>
- +<li><p>neutral AP view (<a href="/articles/shoulder-ap-glenoid-view">Grashey view</a>) and <a href="/articles/axillary-views">axillary views</a> obtained</p></li>
- +<li><p>>2 mm of lucency around the prosthetic component is concerning for loosening</p></li>
- +<li><p><a href="/articles/scapular-notching">"scapular notching"</a> (erosion of the inferior scapular neck) is suggestive of glenoid component failure</p></li>
- +<li><p><a href="/articles/periprosthetic-fracture">periprosthetic fractures</a> at the base of the acromion at the scapular spine are more common</p></li>
- +</ul><h5>CT</h5><ul>
- +<li><p>better for evaluation if there is a suboptimal radiograph</p></li>
- +<li><p>as on conventional radiography, >2 mm of lucency around the prosthetic component is concerning for loosening</p></li>
- +</ul><h5>MRI</h5><ul><li><p><a href="/articles/metal-artifact-reduction-sequence">metal artifact reduction techniques</a> have improved the ability to image prostheses on MRI</p></li></ul><h5>Ultrasound</h5><ul>
- +<li><p>useful for imaging the rotator cuff musculature, evaluating the prosthesis dynamically, and evaluating for joint effusion</p></li>
- +<li><p>cannot be used to evaluate for component loosening</p></li>
- +</ul><h4>Complications</h4><p>The overall complication rate for all forms of total shoulder arthroplasty is ~15%. Complications include:</p><ul>
- +<li><p>aseptic loosening of the glenoid component: most common complication (~30% of all shoulder replacements, but decreased with reverse total shoulder replacements <sup>5</sup>)</p></li>
- +<li><p>aseptic loosening of the humeral component</p></li>
- +<li><p>dislocation</p></li>
- +<li><p>periprosthetic fractures</p></li>
- +<li><p><a href="/articles/acromial-and-scapular-spine-fractures-after-reverse-total-shoulder-arthroplasty" title="Postoperative acromial fractures following reverse total shoulder arthroplasty">acromial/scapular spine fracture</a>, most commonly a stress fracture <sup>6</sup></p></li>
- +<li><p>hardware failure</p></li>
- +<li><p>axillary nerve palsy</p></li>
- +<li><p>infection (uncommon)</p></li>
References changed:
- 6. Lau S & Large R. Acromial Fracture After Reverse Total Shoulder Arthroplasty: A Systematic Review. Shoulder Elbow. 2020;12(6):375-89. <a href="https://doi.org/10.1177/1758573219876486">doi:10.1177/1758573219876486</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/33281942">Pubmed</a>
Image 10 X-ray (Frontal) ( create )