In recent years 4D-CT has emerged as a useful imaging technique in the work-up of patients with primary hyperparathyroidism to allow sensitive detection and localization of parathyroid adenomas and parathyroid hyperplasia.
What is 4D-CT?
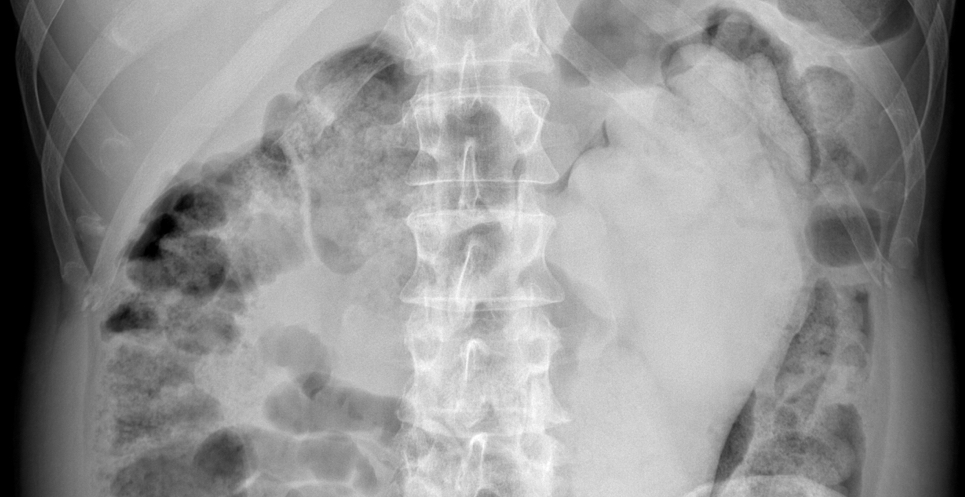
4D-CT includes image sets in three planes (axial, coronal, sagittal) from the angle of mandible to the mediastinum (1). The “fourth” dimension of 4D-CT is the perfusion information derived from multiple contrast phases. It is most commonly performed with three phases: non-contrast, arterial, and delayed phase imaging (1, 2).
Findings of adenoma or hyperplasia
An oval shaped enhancing mass with low attenuation on non-contrast phase relative to thyroid, greatest attenuation in the arterial phase, and rapid washout of contrast in the delayed phase. There are variations in enhancement patterns and helpful morphological findings such as the polar vessel (1, 3, 4).

Do I really need all those imaging phases?
At least 3 phases are required because:
- Only 19% of parathyroid lesions are higher attenuation than thyroid on arterial phase. Other lesions (such as the imaging example here) could be missed without delayed and non-contrast phases (5).
- 23% of adenomas have the similar enhancement to the thyroid on both arterial and delayed phase and could be missed without the non-contrast imaging (5).
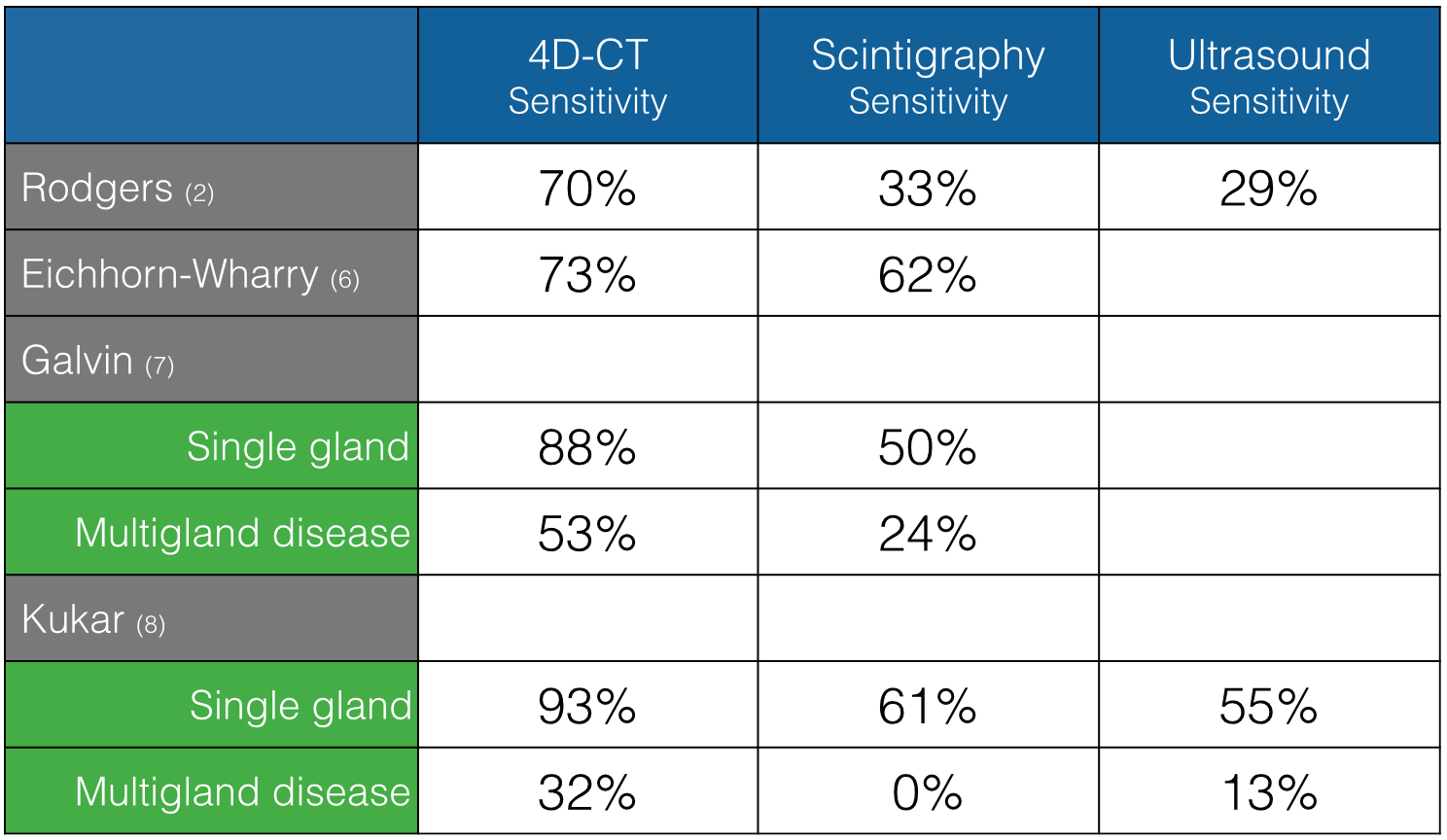
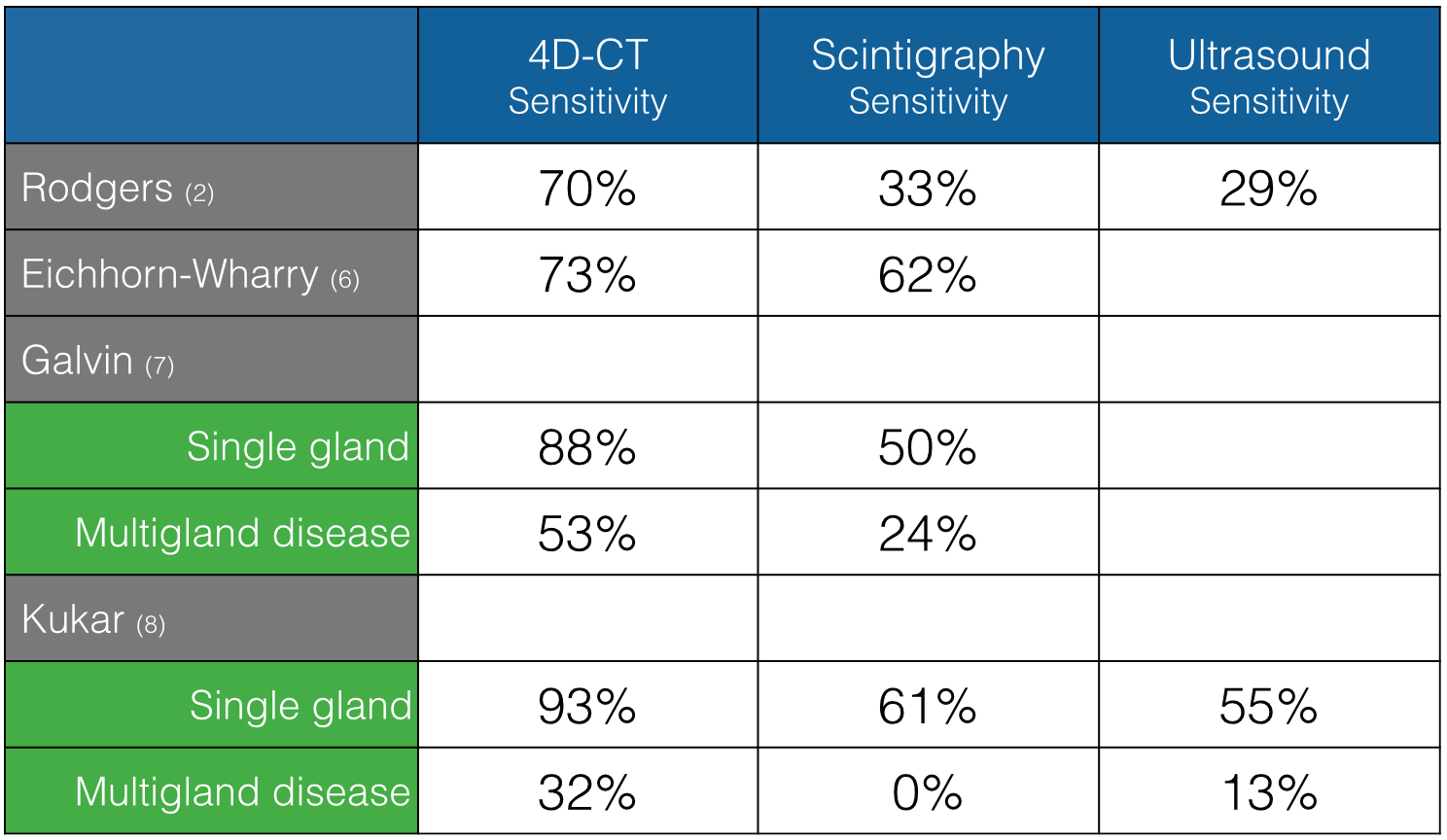
How does 4D-CT compare to scintigraphy and ultrasound?
Several studies have found superior sensitivity of 4D-CT over scintigraphy in the workup of primary hyperparathyroidism.
Other advantages:
-
Difficult subgroups - 4D-CT is superior for subgroups of patients with small lesions, lesions in ectopic sites and multigland disease (2, 7, 8).
-
Surgical planning - 4D-CT assists with surgical planning by providing high-resolution images in multiple planes. The size of the adenoma, polar vessel to the adenoma and surrounding structures are better seen on CT than other modalities. These are all important information for planning minimally invasive surgery.
-
Grading diagnostic confidence – Rather than just stating a study is positive or negative, a combination of imaging findings allows radiologists to provide an estimation of degree of diagnostic confidence (1, 3-5). Diagnostic confidence has become increasingly important in pre-operative planning for minimally invasive parathyroidectomy, in which all four parathyroid glands are not visualized intra-operatively. High diagnostic confidence on 4D CT may also obviate the need for additional imaging, thereby reducing the cost of diagnostic evaluation.
-
Cost-effective – Two studies using decision models have shown that the use of 4D-CT as a second line investigation after traditional modalities fail to localize the lesion is more cost-effective than other imaging protocols (single modality or combination of ultrasound and scintigraphy) (9, 10). This finding is due to the fact that improved localization allows minimally invasive surgery to be performed which is a less costly treatment than bilateral neck exploration and failed surgery.
What about the risk from radiation exposure?
4D-CT has higher radiation dose than scintigraphy, but patients who develop primary hyperparathyroidism have a mean age in the 5th and 6th decades of life and have a lower risk for stochastic effects from radiation exposure (11, 12). A study comparing radiation dose from 4D-CT to scintigraphy found the effective dose was 28 mSv for 4DCT compared to 12 mSv for scintigraphy (13). However, in the exposed standard patient (female of 55 years age), the increase in lifetime incidence of cancer over baseline cancer risk was extremely small at 0.52% for 4DCT and 0.19% for scintigraphy. Given both studies cause negligible increases in lifetime risk of cancer, clinicians should not allow concern for radiation-induced cancer influence decisions regarding workup in older patients.

|
Dr Jenny Hoang, MBBS FRANZCR
Associate Professor of Radiology and Radiation Oncology at Duke University Medical Center in Durham NC, United States of America. Dr Hoang has particular expertise in the area of parathyroid imaging and has produced several published and in press papers related to this topic. Connect with her via twitter @JennyKHoang.
|
REFERENCES
1. Hoang JK, Sung WK, Bahl M, Phillips CD. How to Perform Parathyroid 4D CT: Tips and Traps for Technique and Interpretation. Radiology. 2014;270(1):15-24.
2. Rodgers SE, Hunter GJ, Hamberg LM, Schellingerhout D, Doherty DB, Ayers GD, Shapiro SE, Edeiken BS, Truong MT, Evans DB, Lee JE, Perrier ND. Improved preoperative planning for directed parathyroidectomy with 4-dimensional computed tomography. Surgery. 2006;140(6):932-40; discussion 40-1.
3. Bahl M, Muzaffar M, Vij G, Sosa JA, Choudhury KR, Hoang JK. Prevalence of the polar vessel sign in parathyroid adenomas on the arterial phase of 4D CT. AJNR American journal of neuroradiology. 2014;35(3):578-81.
4. Bahl M, Sepahdari A, Sosa JA, Hoang JK. Parathyroid Adenomas and Hyperplasia on 4DCT: Different Enhancement Patterns Illustrate Importance of Multiple Phases. Under review. 2014.
5. Bahl M, Sepahdari A, Sosa JA, Hoang JK. Parathyroid Adenomas and Hyperplasia on 4D CT: Grading System for Degree of Confidence. RSNA Oral Scientific Presentation. 2014.
6. Eichhorn-Wharry LI, Carlin AM, Talpos GB. Mild hypercalcemia: an indication to select 4-dimensional computed tomography scan for preoperative localization of parathyroid adenomas. American journal of surgery. 2011;201(3):334-8; discussion 8.
7. Galvin P, Oldan J, Bahl M, Sosa JA, Hoang JK. Discordant Parathyroid 4DCT and Scintigraphy Results: What Factors Contribute to Missed Parathyroid Lesions? Oral scientific presentation at ASNR Montreal 2014. Under review for publication. Oral Scientific presentation at the American Society of Neuroradiology Scientific Meeting. Montreal, Canada 2014.
8. Kukar M, Platz TA, Schaffner TJ, Elmarzouky R, Groman A, Kumar S, Abdelhalim A, Cance WG. The Use of Modified Four-Dimensional Computed Tomography in Patients with Primary Hyperparathyroidism: An Argument for the Abandonment of Routine Sestamibi Single-Positron Emission Computed Tomography (SPECT). Ann Surg Oncol. 2014.
9. Wang TS, Cheung K, Farrokhyar F, Roman SA, Sosa JA. Would scan, but which scan? A cost-utility analysis to optimize preoperative imaging for primary hyperparathyroidism. Surgery. 2011;150(6):1286-94.
10. Lubitz CC, Stephen AE, Hodin RA, Pandharipande P. Preoperative localization strategies for primary hyperparathyroidism: an economic analysis. Ann Surg Oncol. 2012;19(13):4202-9.
11. Yeh MW, Ituarte PH, Zhou HC, Nishimoto S, Liu IL, Harari A, Haigh PI, Adams AL. Incidence and prevalence of primary hyperparathyroidism in a racially mixed population. J Clin Endocrinol Metab. 2013;98(3):1122-9.
12. Wermers RA, Khosla S, Atkinson EJ, Achenbach SJ, Oberg AL, Grant CS, Melton LJ, 3rd. Incidence of primary hyperparathyroidism in Rochester, Minnesota, 1993-2001: an update on the changing epidemiology of the disease. J Bone Miner Res. 2006;21(1):171-7.
13. Hoang JK, Reiman RE, Nguyen GB, Januzis N, Chin BB, Lowry C, Yoshizumi TT. Lifetime Attributable Risk of Cancer from Radiation Exposure During Parathyroid Imaging: Comparison of 4DCT and Parathyroid Scintigraphy. In press. AJR 2015.
 Dr Henry Knipe is a radiology registrar at The Royal Melbourne Hospital in Australia, and is managing editor responsible for content development at Radiopaedia.org. Twitter: @DrHenryK.
Dr Henry Knipe is a radiology registrar at The Royal Melbourne Hospital in Australia, and is managing editor responsible for content development at Radiopaedia.org. Twitter: @DrHenryK.













 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.