Presentation
Epigastric pain, acute onset, radiating to the back. Vomiting. Started pegaspargase 2 weeks prior for acute lymphoblastic leukaemia.
Patient Data

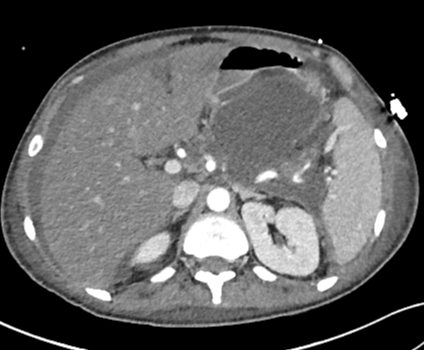
The pancreas is enlarged and heterogeneous. There is abnormal fluid attenuation in the retroperitoneum and a small volume of ascites.
In the context the appearances are in keeping with acute pancreatitis.
The majority of the pancreas has been replaced by a large fluid collection, with only a small part of the head of the pancreas demonstrating enhancement. There is a small volume of ascites. There is a filling defect in the splenic vein.
The appearances are in keeping acute necrotising pancreatitis with associated splenic vein thrombosis.
Case Discussion
The imaging demonstrates acute pancreatitis secondary to pegaspargase, a drug used to treat acute lymphoblastic leukaemia. A diagnosis of acute pancreatitis can be made in the presence of 2 of the three conditions 1:
abdominal pain suggestive of pancreatitis
serum amylase or lipase >3 times the upper limit of normal
characteristic imaging findings of pancreatitis
In this case, because pancreatitis was not suspected clinically, serum amylase/lipase were not obtained prior to imaging. They were subsequently measured and found to be >3 times the upper limit of normal.
In cases where CT is obtained early in acute pancreatitis (< 2 days after the onset of pain), the initial CT can fail to detect the degree of pancreatic necrosis, as in this case. The subsequent CT at 9 days after the onset of pain demonstrates extensive pancreatic necrosis, involving almost the entire pancreas.
The learning points here are:
serum amylase / lipase should be obtained prior to imaging where acute pancreatitis is in the differential
if they are elevated, in almost all cases it is appropriate to avoid images with CT in the first 2 days
CT < 2 days after the onset of pain can fail to detect the degree of pancreatic necrosis




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.