Presentation
Chills, profuse sweating, intermittent fevers, fatigue and nausea with no history of trauma or surgery.
Patient Data




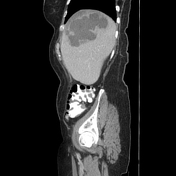

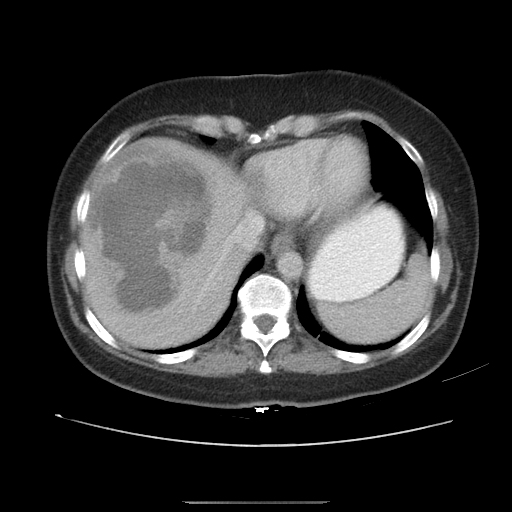
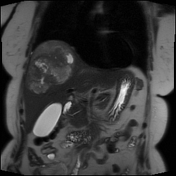
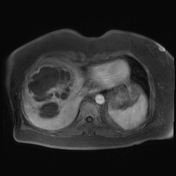
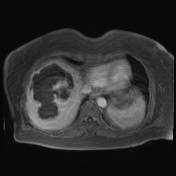
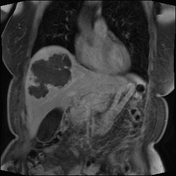
CT of the abdomen and pelvis with IV and oral contrast shows an irregular peripherally enhancing lesion in the right hepatic lobe, extending to the hepatic dome. There is oedema around the lesion, suggestive of a "double target sign". This is a large single lesion. No other lesion is seen in the abdomen or pelvis. There is colonic diverticulosis without acute diverticulitis. No colonic wall thickening or pericolic fat stranding is seen to suggest colitis.












MRCP: biliary tract appears normal without evidence of cholangitis
MRCP: pancreatic divisum
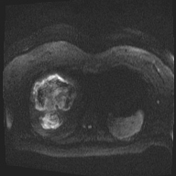
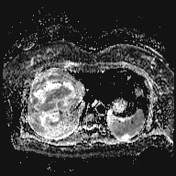
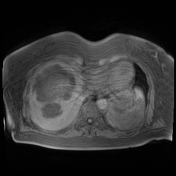
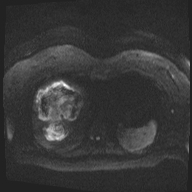
DWI/ADC: areas of diffusion restriction in the lesion
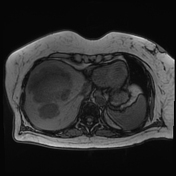
T2: heterogeneous signal in the lesion
post-contrast: peripheral enhancement without internal enhancement
this is a single lesion with multiple lobulations and irregular margins
no lymphadenopathy or perihepatic fluid
motion artifact in the phase-encoding direction
Patient lab values:
WBC count: 15.5 K/UL
Alkaline phosphatase: 281 U/L
ALT: 71 U/L AST: 97 U/L
Case Discussion
Abdominal CT and MRI showed a non-enhancing lesion in the right hepatic lobe consistent with a large fluid collection, with no solid component to suggest malignancy. A percutaneous hepatic drainage catheter was placed by interventional radiology. Purulent fluid was obtained. Cytology was negative for malignancy. Standard cultures were negative, and parasitic infections were considered due to recent travel to Mexico. A positive Entamoeba histolytica antibody confirmed the diagnosis of an amebic liver abscess. The patient was treated with ceftriaxone/metronidazole. The abscess resolved on follow-up imaging and the drain was removed 1 month after it was placed.
The patient's clinical history and imaging features should raise suspicion for atypical infection. The antibody test may take several days to result, and therefore antibiotic treatment may initially be guided by the differential diagnosis on imaging.
Case co-author: Sanika Patil, MD (Loyola University Medical Centre)




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.