Presentation
4-5 days of increasing right knee pain with limp and fevers
Patient Data



Normal alignment of the knee joint. No fracture or joint effusion.
No fracture or radiographic features of osteomyelitis or septic arthritis.











Marrow oedema with heterogeneous enhancement of the proximal tibial metaphysis (coronal, axial). There is periosteal reaction medially (coronal, axial) .
Patchy marrow oedema also noted in the posterior proximal epiphysis (coronal, axial).
No intraosseous or soft tissue collection. No knee joint effusion. Preserved femoral marrow signal.
Findings are suspicious for osteomyelitis of the right proximal tibia.




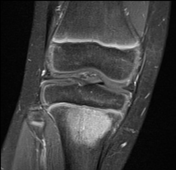








A new, well-circumscribed and peripherally enhancing lesion is situated at the mid-posterior physis of the proximal tibia. It is T1 hypointense and T2 hyperintense relative to adjacent marrow, memasuring 10 x 10 x 5 mm.
The region of epiphyseal marrow oedema has increased and now extends into the physis, and is more hypointense on T1- and hyperintense on T2-weighted imaging than previous.
Compared to the core, the lesion rim is slightly hyperintense on T1-weighted imaging with post-contrast enhancement, consistent with the penumbra sign.
The circumscribed lesion and surrounding oedema do not extend to the joint surface.
No evidence of sequestrum, involucrum or cloaca. No soft tissue collection or evidence of sinus tract. No synovitis or joint effusion is seen.
Conclusion
Findings are consistent with the interval development of Brodie abscess in the context of subacute osteomyelitis. No other complications of acute or chronic osteomyelitis are seen.
Case Discussion
This otherwise healthy 9-year-old boy presented with 4-5 days of fevers, right knee pain and inability to weight bear. There was no history of trauma.
The child examined well. He was happy and not in pain at rest. There was only minimal tenderness to the joint on palpation. He had no joint effusion clinically.
He had a CRP of 46 mg/L but no leucocytosis. A plain film of the knee was unremarkable. Ultrasound of the knee did not demonstrate effusion or hyperaemia.
He was admitted to hospital for an MRI and empiric osteomyelitis treatment with IV flucloxacillin, but his pain and limp did improve.
Repeat MRI 6 days later showed findings consistent with Brodie abscess with a positive penumbra sign. Blood cultures remained negative and serology was negative for tuberculosis.
He was managed conservatively with 2 weeks of IV antibiotics and was discharged home after his limp resolved and repeat MRI showed no further signs of abscess. He continued 6 weeks of broad-spectrum antibiotics in the community.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.