Presentation
Transferred from another hospital. Presented with severe abdominal pain and distension.
Patient Data
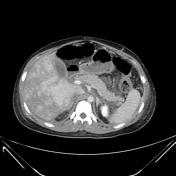






Small right pleural effusion.
Distended azygous vein.
Non-opacified retrohepatic IVC with central low attenuation.
Hepatomegaly.
Heterogeneous hepatic enhancement.
Moderate ascites with left flank drain.

Further dilatation of the azygous vein.
Patent transjugular intrahepatic portosystemic shunt (TIPS) between the portal vein and the proximal IVC.
Similar size liver with more homogeneous enhancement.
Interval splenic enlargement.
Minor pelvic ascites.













Multiple enhancing lesions throughout both lobes of the liver, particularly involving the right lobe. The largest lesion is seen in segment 4b measuring 26 x 24mm.
The lesions are arterially enhancing with persistent enhancement on the portal venous and hepatobiliary phase.
Several of the lesions demonstrate rim enhancement, and have rim uptake on the hepatobiliary
phases.
No diffusion restriction (not shown).
Lesions are low signal intensity or difficult to identify on T2-weighted imaging however the largest lesions demonstrates heterogeneous hyperintensity. Most of the lesions are T1 hyperintense.
There is no intrahepatic biliary dilatation.
TIPS noted between the middle hepatic vein region and the confluence of the portal veins.
Portal vein is patent and of normal calibre.
Patchy enhancement of the liver with reduced peripheral enhancement.
Hepatic veins are markedly narrowed and do not enhance.
Splenic size at the upper limit of normal.
No ascites. No portal adenopathy.
CONCLUSION:
Multiple arterially enhancing lesions with continued enhancement on the portal and delayed phases, with retention of contrast medium on the hepatobiliary phase. In the setting of Budd-Chiari these are consistent with large regenerative nodules (FNH-like lesions).
Case Discussion
The initial presentation was Budd Chiari syndrome (hepatic veno-occlusive disease), spontaneous bacterial peritonitis (Neisseria meningitidis), lower limb DVT and pulmonary embolism. She was diagnosed and treated for paroxysmal nocturnal haemoglobinuria. Her high LDH and reticulocytosis are indicators for intravascular haemolysis and her high LDH is a risk factor for thromboembolism 1. Her IVC and hepatic vein thrombosis was unresponsive to anticoagulants and the resulting portal hypertension was managed with transjugular intrahepatic portosystemic shunt.
Clone size was 98%. She was successfully treated with infusions of ecluzimab and oral rivaroxiban. She later suffered a further episode of meningococcal sepsis.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.