Presentation
The patient presents with dysuria, pyuria, fever, and intermittent urinary retention. There is no significant past or known medical history specifically there is no diabetes mellitus or previous pulmonary tuberculosis.
Patient Data
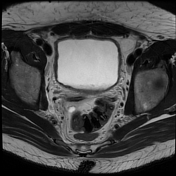

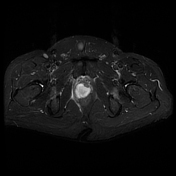

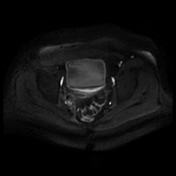

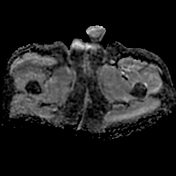





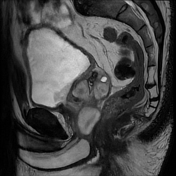

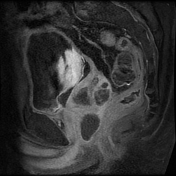

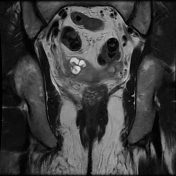

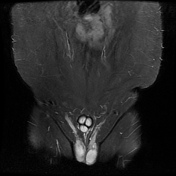

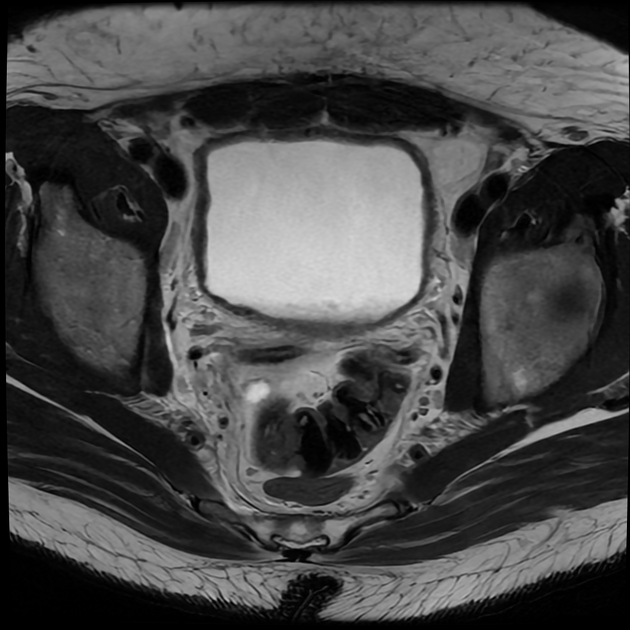
Features suggestive of a disseminated or complicated urinary tract infection with cystitis, seminal vesiculitis, prostatitis with prostatic abscesses, vasitis, urethritis, and regional colitis.
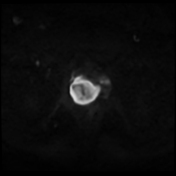
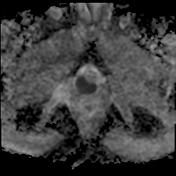
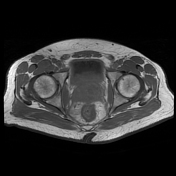
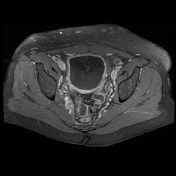
This is demonstrated by the distended urinary bladder with intracystic sedimented debris. There is prostatitis complicated by multiple macro and microcystic intraprostatic abscesses, of varying sizes involving the entire prostate from the base to the apex and within both the peripheral and transitional zones. There is heterogeneous seminal vesicle signal intensity with some left-sided desiccation. There is a variable restriction on diffusion imaging of the bladder wall, the bladder sedimented debris, prostate, and abscess contents, the seminal vesicles, bilateral vas deferens, and to a certain extent the regional colonic wall and urethra.
There is the expected abnormal bladder wall, seminal vesicles, vas deferens, and colonic wall enhancement on contrast administration. There is irregular and ringlike prostatic abscess wall enhancement. Suspected normal enhancement within the corpora cavernosa bilaterally. There is abnormal urethral enhancement post-contrast administration.
There are no necrotic intrapelvic or inguinal lymph nodes. Shotty inguinal lymph nodes which enhance on contrast administration.
There is no pelvic osteomyelitis or septic arthritis.
Case Discussion
An example of a severe lower urinary tract infection with cystitis and pyuria, prostatitis and multiple prostatic abscesses, seminal vesiculitis, vasitis, urethritis, and regional colitis.
The patient was referred for admission and further work-up to determine the source of the sepsis. Transrectal ultrasound-guided aspiration was also envisaged.
Escherichia and Staphylococcus infections were the considered working diagnosis. Urogenital tuberculosis was considered less likely due to a known immune competence, ie. the patient was HIV-negative.
Unfortunately, the patient opted for treatment at an external facility and we were unable to confirm a final diagnosis.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.