Presentation
Interhospital transfer following high velocity rope strangulation. Carotid injury requiring stenting. Difficult ventilation.
Patient Data
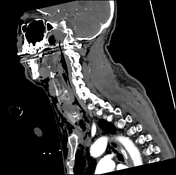












Right CCA stent extending into the proximal right ICA is patent. Right ACA and MCA are patent. The left CCA remains occluded shortly after its origin with a thin column of contrast seen in the proximal cervical and petrous segments of the left ICA. No contrast evident in the remainder of the left ICA. The left ACA and MCA are well opacified likely from flow via the Acom artery. Vertebral, basilar, and posterior cerebral arteries remain patent. The jugular veins are poorly opacified due to the phase of contrast.
The balloon of the ETT is inflated within the cervical trachea 29 mm below the cricoid arch and 50 mm above the carina. In the midline there is a large contiguous locule of gas extending inferiorly from the larynx anterior to the ETT underneath the cricoid arch in keeping with at least partial rupture of the cricotracheal ligament. The cricoid arch and lamina appear intact (noting incomplete calcification).
Extensive pneumomediastinum and subcutaneous emphysema is again demonstrated. Gas dissects into bilateral pleural spaces with small bilateral pneumothoraces anteriorly.
Normal alignment of cervical spine. No cervical spine fracture identified. Orogastric tube extends below the field of view.
Impression
Patent right CCA stent. Improved flow within the right ICA compared to pre procedure CT.
Left CCA and the majority of the left ICA remain occluded.
Bilateral ACAs and MCAs are patent with the left anterior circulation likely supplied by the Acom artery.
Rupture of the cricotracheal ligament causing cricotracheal separation.
Extensive subcutaneous emphysema, pneumomediastinum, and small bilateral pneumothoraces.



Large contiguous locule of gas extending inferiorly from the larynx anterior to the ETT underneath the cricoid arch in keeping with at least partial rupture of the cricotracheal ligament.
Case Discussion
The patient went to theatre where the ENT team performed direct laryngoscopy, flexible bronchoscopy and microlaryngoscopy which identified a 2 cm anterior defect from the subglottis to the first tracheal ring. Repeat assessment one week later showed granulation tissue covering the defect.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.