Presentation
Headache, fever, fatigue, and neck stiffness. Blood tests show an elevated white blood cell count and an increased percentage of eosinophils.
Patient Data
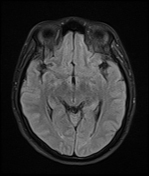

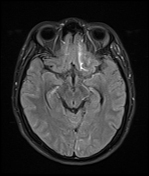

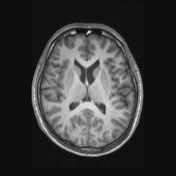

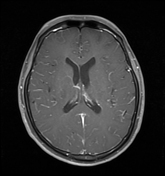

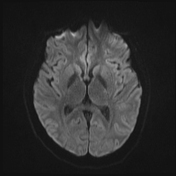

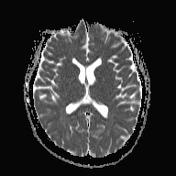

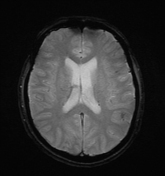



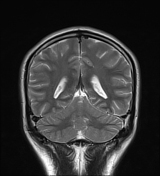

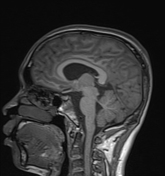

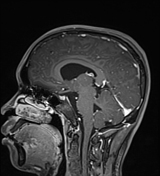

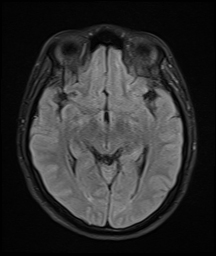
MRI shows no evidence of brain parenchyma lesions. Pre-contrast sequences show no significant signal abnormalities. On FLAIR and T1FS post-contrast, there is increased signal in the sulci of both cerebral hemispheres, indicative of leptomeningeal thickening and enhancement.
The patient underwent a lumbar puncture and the tests yielded the following results:
clear, colorless fluid, with a rate of 100-120 drops per minute
cytology: red blood cells 336 cells/mm³, white blood cells 371 cells/mm³, neutrophils 35%, lymphocytes 54%
glucose: 2.8mmol/L (normal 2.5 - 4.5)
lactate: 2.1 mmol/L (normal 0.5 - 2.2)
protein: 0.58 g/L (normal 0 - 0.3)
real-time PCR (for multiple bacterial pathogens causing meningitis): negative
real-time PCR (for multiple viral pathogens causing meningitis): negative
direct AFB staining with Ziehl-Neelsen: negative
direct microscopy for fungi: negative
mycobacterium tuberculosis identification and RMIP resistance by Xpert: no tuberculosis bacteria detected
Blood tests show a white blood cell count of 14.7 G/L, eosinophils at 24.8%, and CRP at 15.4 mg/L.
Strongyloides stercoralis (threadworm) Ab automated immunoassay: positive.
Stool examination for ova and parasites: negative.
Case Discussion
Imaging, clinical, and laboratory findings are consistent with eosinophilic meningitis.
The patient was subsequently treated with antiparasitic medication (albendazole) and corticosteroids (dexamethasone). Clinical symptoms improved and blood tests returned to normal, indicating a response to treatment.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.