Presentation
The patient noted left-sided upper extremity weakness and a downturned left mouth angle two hours before admission to the emergency room.
Patient Data
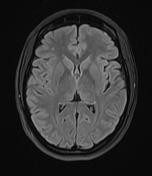








Urgent MRI shows no abnormalities on FLAIR, except few punctiform, nonspecific hyperintensities in the white matter. DWI and ADC map show areas of restricted diffusion in right frontal and insular lobes, in accordance with a hyperacute ischaemia. Time of flight angiography (TOF) shows no flow detected in insular and cortical frontal branches of right middle cerebral artery, indicating thrombosis.

The patient underwent an endovascular thrombectomy and showed improvement in symptoms. However, ischaemic area described on the initial MRI is now visible as a demarcated, hypodense area of brain parenchyma with dedifferentiation of gray and white matter, in accordance with acute ischaemia.
Case Discussion
The patient presented to the emergency room (ER) two hours after the onset of symptoms. The attending neurologist's report noted no nausea or vomiting. No recent trauma or loss of consciousness. No significant prior medical history was noted.
The patient was conscious, orientated, understood questions, and followed commands, with normal speech expression. The pupils were isocoric, and photomotor function was normal. The eye globes were in an orthoposition, bulbar motor function was normal, and no nystagmus was observed. The patient denied diplopia. The visual field appeared normal. A supranuclear lesion of the facial nerve was noted on the left. The tongue protruded midline. No signs of meningeal irritation were present. In the anti-gravity position, the left arm drifted down towards the surface, while the other extremities were able to be brought to and held in the anti-gravity position. Myotatic reflexes were symmetric, graded 2+, and pathological reflexes were not elicited. No sensory deficits were reported. The patient was examined while lying down. No signs of urinary or bowel incontinence were noted. The patient was afebrile, with no signs of heart failure, and normal respiratory function was observed.
An urgent MRI is a valuable tool in the diagnosis of hyperacute stroke. Diffusion-weighted imaging (DWI) is the most sensitive and specific imaging technique for the diagnosis of acute ischaemia, even in a hyperacute setting. Treatment options include intravenous thrombolysis and mechanical thrombectomy. For both options, the time at which treatment is initiated is crucial ("time is brain") - greater benefits are observed if treatment is delivered within 4.5 hours of symptom onset. Good collateral circulation is also beneficial. It is important to know that for every hour of delay, parenchymal reperfusion decreases by 20%.
In our case, the attending radiologist opted for an urgent MRI rather than a CT scan due to the short time interval between symptom onset and admission to the ER, which corresponded with the hyperacute phase of stroke, likely making it not visible on a CT scan. MRI confirmed hyperacute ischaemia of the brain and detected a lack of flow in the corresponding right middle cerebral artery branches. The patient was administered intravenous thrombolysis treatment and referred to a national stroke centre at a nearby hospital, where mechanical thrombectomy was performed with an improvement in the patient's symptoms.
Timely diagnosis and the selection of an optimal imaging modality are crucial for the successful treatment of stroke patients.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.