Presentation
The patient presents with dull, persistent lower abdominal pain. Ultrasound findings suggest a tumour in the right ovary and a corpus luteum cyst in the left ovary.
Patient Data
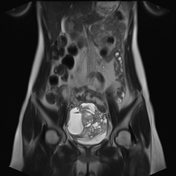

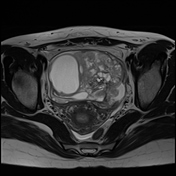

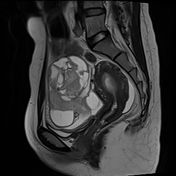

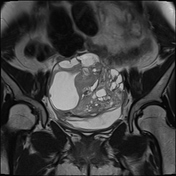

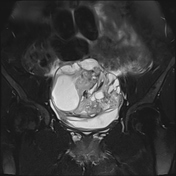

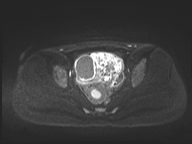

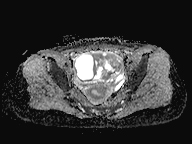

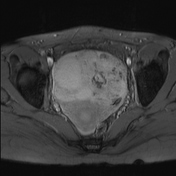

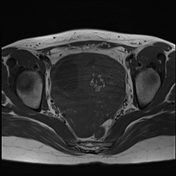

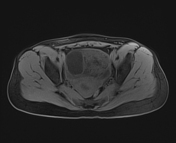

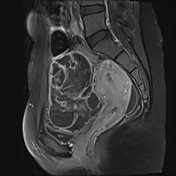

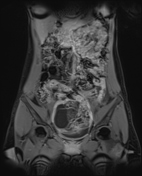

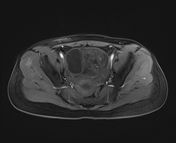

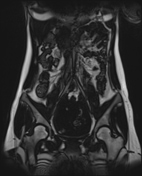

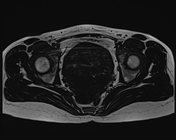

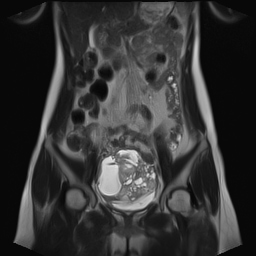
A mixed lesion in the lower abdomen, measuring 95 x 71 x 83 mm (width x anteroposterior x height), with heterogeneous signals comprising solid, cystic components, multiple septations, and calcifications/haemorrhage scattered inside. The lesion has unclear borders, partially merging with the right ovary. The signal is mainly intermediate to high on T2TSE, low to intermediate on T1TSE, partially low on GRE, with scattered restricted diffusion. There is strong, heterogeneous enhancement of the solid components and septations after contrast injection. The lesion compresses surrounding structures. No signs of torsion or rupture of the tumour. No suspicious pelvic lymph nodes observed.
The left ovary measures 31 x 21 mm, with multiple small unilocular cysts <3 cm at the periphery, likely follicular cysts, and a 13 mm cyst with thickened, irregular walls and peripheral enhancement, suggestive of a corpus luteum cyst.
Fluid collection in the Douglas pouch, measuring 13 mm.
Blood test:
CA 125 (Cancer Antigen 125) level: 45.81 U/mL (normal)
HE4 (Human Epididymal Protein 4) level: 55.31 pmol/L (normal)
AFP (Alpha Fetoprotein) level: 28.3 ng/mL (elevated)
bhCG (Beta Human Chorionic Gonadotropin) level: 0.27 mU/mL (normal)
Surgical report:
abdominal cavity: approximately 20 ml of pinkish fluid observed
right ovary: a 10 x 10 cm mass, intact with no rupture, no vascular proliferation, and no surface excrescences
left ovary: a 2 x 3 cm cyst, resembling a corpus luteum cyst
the tumour was completely excised and sent for immediate frozen section biopsy, which confirmed malignancy. The right adnexectomy and the ovarian tumour were sent for histopathological examination
left ovarian cyst excision was performed, and the specimen was sent for histopathological examination. The uterus and left adnexa were preserved
laparoscopic omentectomy was performed, and the specimen was sent for histopathological examination
Macroscopic:
The specimen consists of an ovary measuring 5.5 x 4.5 cm, presenting as a thin-walled cyst, along with a fallopian tube measuring 7 x 1 cm. The external surface is light brown, and the cut surface is soft.
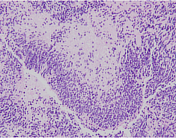
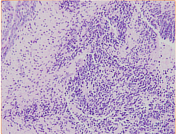
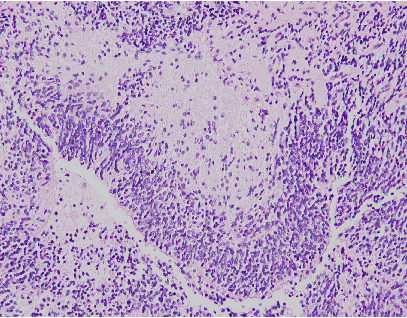
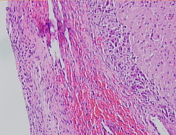
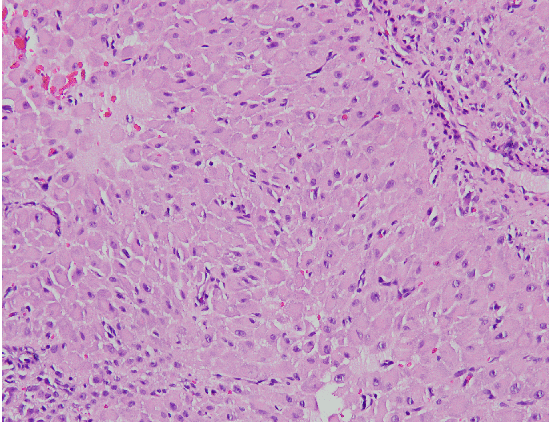
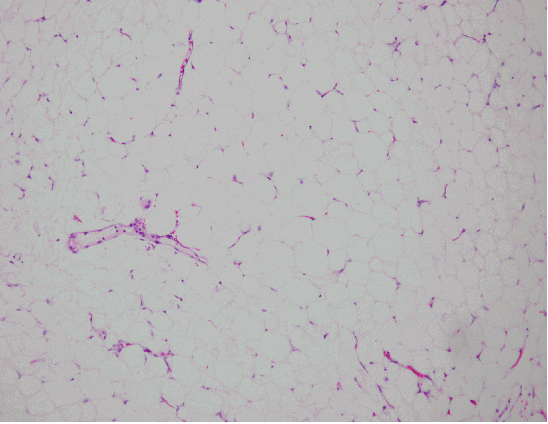
Microscopic:
The tumour structure includes components from all three germ layers, with the presence of immature neural epithelium in ≤ 3 low-power fields, showing neural tube-like structures.
Conclusion:
Immature teratoma, grade 2.
Macroscopic:
The specimen consists of a single sample measuring 1.5 x 1 cm, light brown in colour with a soft cut surface.
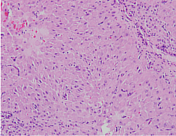
Microscopic:
The structure shows a haemorrhagic cyst interspersed with clusters of luteinized cells.
Conclusion:
Haemorrhagic corpus luteum cyst of the ovary.
Macroscopic:
One sample, measuring 40 x 10 cm, light yellow in colour, with no discernible lesions.
Microscopic:
The biopsy sample consists of fibrous connective tissue and adipose tissue, with no abnormal findings.
Conclusion:
Fibrous connective tissue and adipose tissue, no malignant features observed.
Case Discussion
Imaging findings, surgical observations, blood tests, and histopathological examination confirm the diagnosis of immature ovarian teratoma.
In this case, the MRI shows several features suggesting a high risk of malignancy (O-RADS 4), including:
a mixed composition (solid and cystic) with heterogeneous signals
areas of necrosis or haemorrhage, low signal intensity on GRE
the mass exhibits high signal intensity on T2W, low signal intensity on T1W, and restricted diffusion (due to solid tissue or immature neural tissue)
the typical macroscopic fat signal seen in mature teratomas is often absent
thick, irregular septations
enhancement with contrast, comparable to the myometrium, is observed in the solid components and septations
Case co-author: Consultant specialist Tran Quyet Thang, Military Hospital 175, Vietnam.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.