Presentation
Asymptomatic male.
Patient Data

The Inferior vena cava pictured in the cine-loop demonstrates respirophasic changes in a spontaneously breathing patient
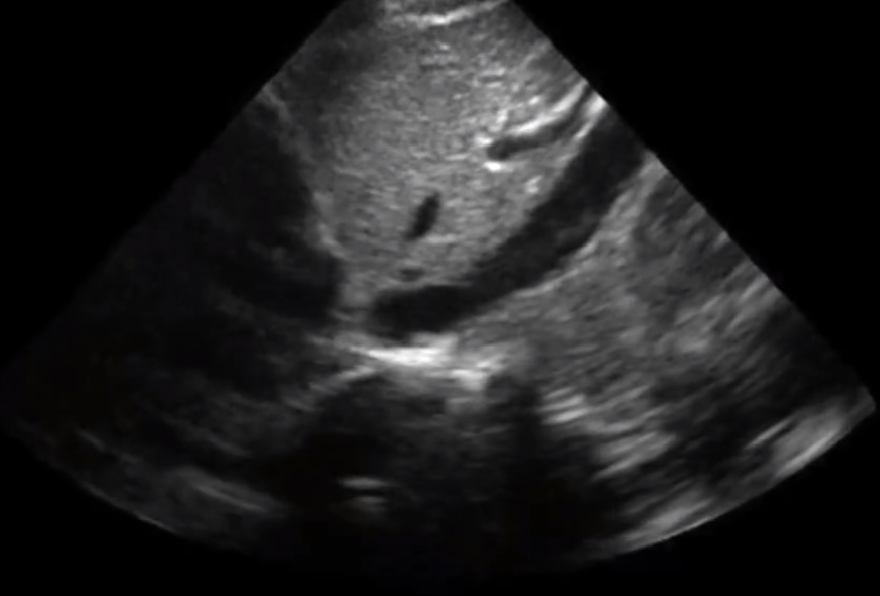
The annotated still image depicts a nearly fully collapsed Inferior vena cava (red arrows)
Case Discussion
Ultrasonographic measurement of inferior vena cava (IVC) diameter and degree of respirophasic collapse was initially utilised by nephrologists and subsequently cardiologists. It has more recently been integrated into several critical care/emergency ultrasound protocols as a non-invasive estimate of central venous pressure (CVP).
Considerable heterogeneity exists among authors regarding the exact relationship between Right atrial pressure and the behaviour of the IVC; the American Society of Echocardiography recommends that the following specific values be used when guiding interventions:
- maximum size < 2.1 cm and a collapse >50% during sniff = right atrial pressure 0–5 mm Hg
- maximum size > 2.1 cm; collapses >50% during sniff = 5–10 mm Hg
- maximum size > 2.1; collapses <50% during sniff = 10–20 mm Hg
Learning Points:
Baseline diameter of the IVC and the degree of change induced by inspiration are used to calculate the Caval Index, reported as a percentage; a number close to 100% is indicative of almost complete collapse, while a number close to 0% suggest minimal collapse
Caval Index, or IVCC, is performed by calculating the difference between the inspiratory and expiratory diameters, and dividing by the latter (normal >50%).
In the appropriate clinical context, a plethoric IVC with minimal respiratory variation is congruent with elevated filling pressures, while a collapsed slit-like IVC may provide supporting evidence for intravascular volume depletion.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.