Presentation
Recent road traffic accident.
Patient Data
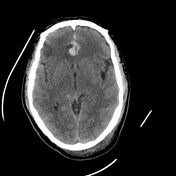

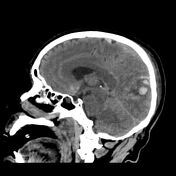



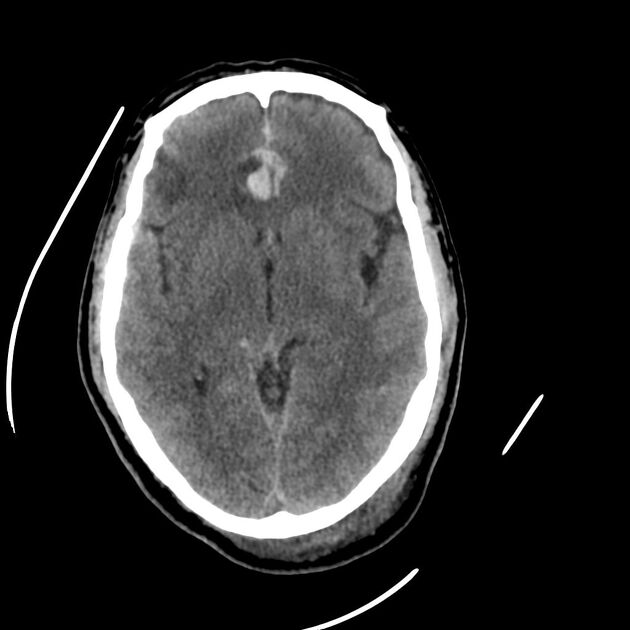
Multiple punctate cortical and subcortical hyperdense areas surrounded by a hypodense halo of oedema involving bilateral frontal, right occipital and left temporal lobes are more evident in the right frontal lobe (acute haemorrhagic contusions). Smearing of cortical sulci of both cerebral hemispheres by linear hyperdensity (acute subarachnoid haemorrhage). Intra-ventricular hyperdense areas within the left lateral ventricle (intra-ventricular haemorrhage). Bi-occipital subgaleal haematoma.
Variable degree of opacification of all paranasal sinuses by hyperdense and isodense fluid (haemosinuses).
Case Discussion
Intracranial haemorrhage (ICH) is a common condition with various causes, including trauma, hypertension, vascular abnormalities, and ischaemic stroke complications. Neuroimaging plays a crucial role in diagnosing the cause, assessing severity, predicting potential brain damage, and guiding urgent treatment 1.
Trauma is the leading cause of ICH, with CT scans being the first-line imaging tool for assessing acute brain injury. However, MRI is increasingly used in emergency settings due to its higher sensitivity in detecting small haemorrhages and axonal injuries. Trauma can cause ICH by damaging arteries and veins beneath the skull, leading to bleeding over or within brain tissue. Common types of traumatic ICH include subarachnoid haemorrhage, epidural and subdural haematomas, haemorrhagic contusions, and cerebral microhaemorrhages from shear injury 1.
Our case shows two main types of the aforementioned intracerebral haemorrhages including the subarachnoid haemorrhage and haemorrhagic contusion in addition to intra-ventricular extension of blood, subgaleal haematoma and haemosinuses.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.