Presentation
First episode of a generalized seizure in a previously healthy patient. Glasgow coma scale score of 15 and normal neurological examination post-seizure. Possible seizure substrate?
Patient Data
ASNR Case of the Day Winner 2022
This case was selected as the winner of the 2022 ASNR Case of the day competition winner. Runner-up and honorable mentions can be viewed in this playlist.
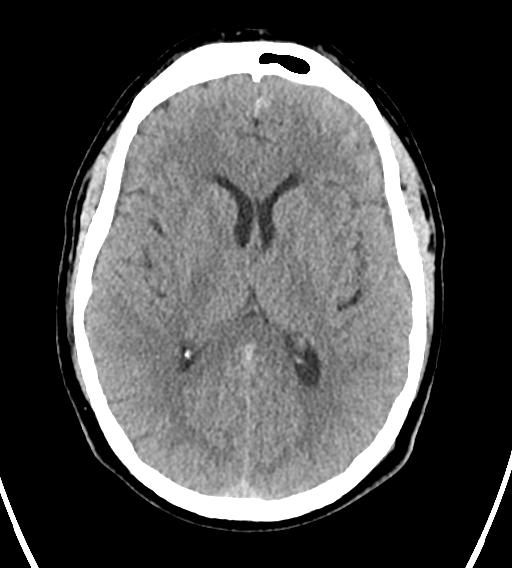
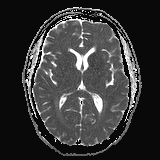
An ill-defined area of gyriform hyperdensity in the inferior right frontal lobe. Several small, subtle areas of hyperdensity overlying the left frontal lobe. Mild diffuse sulcal narrowing involving the left frontal lobe. No intra-axial mass or hydrocephalus.
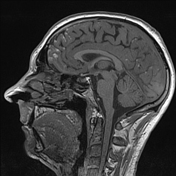

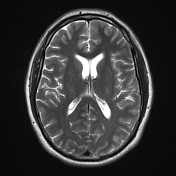

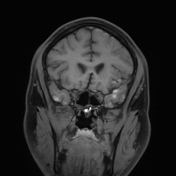

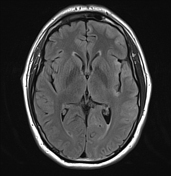

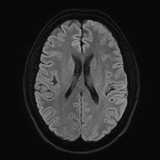


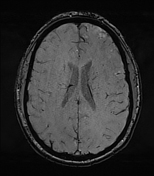

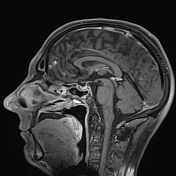

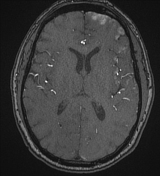

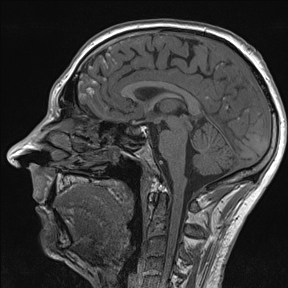
Extensive diffuse nodular areas of high T1 signal on the surface of sulci and gyri predominantly involving the anterior left frontal and temporal lobes. Focal gyriform area of high T1 signal involving the right inferior frontal lobe, which also displays susceptibility artefact suggestive of hemorrhage. Mild sulcal effacement of the left frontal and temporal lobes. Incomplete suppression of CSF signal on FLAIR over the left frontal convexity.
No pachymeningeal enhancement. No ventricular dilatation or ependymal enhancement.
The cerebral arteries are normal in caliber with no aneurysm or vascular malformation.
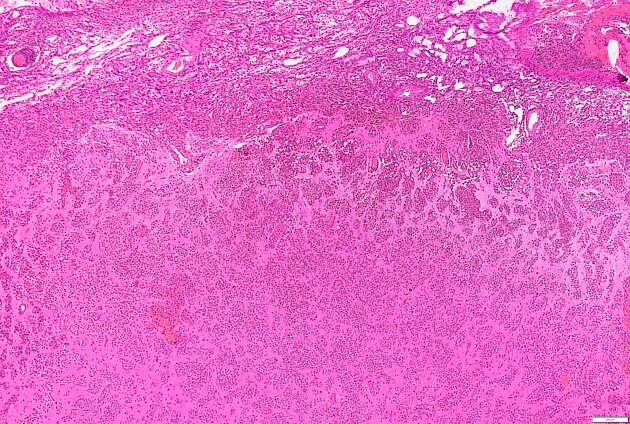
Microscopy: 1. to 3. Biopsies are from one intraoperative lesion and are described together. There is a pleomorphic neoplasm infiltrating the leptomeningeal space and extending into the cortex along Virchow-Robin space (also seen in specimens 2 and focally in specimen 3). The cells show nuclear pleomorphism with eosinophilic nucleoli and cytoplasmic melanin, and form sheet-like nodules with brain invasion. No necrosis is present and mitotic figures are not seen (0/10 HPF). The neoplastic cells express SOX10 and HMB45 (majority of cells). Ki67 proliferation index is estimated at 5%. The neoplasm shows pleomorphic melanocytes with leptomeningeal spread and brain invasion. The features are of leptomeningeal melanomatosis.
Supplementary report: c-Kit staining is positive.
Summary: 1.-3. Cortex, left frontal lobe; Parenchyma, left frontal lobe; Deep lesional tissue - Leptomeningeal melanomatosis, please see description.
Case Discussion
Meningeal melanomatosis is a rare malignant primary melanocytic tumor of the central nervous system, which is thought to originate from malignant transformation of melanocytic precursor cells. It most often occurs in children, where it can be associated with neurocutaneous melanosis, however it can also present in adulthood.
This case demonstrates the importance of careful assessment of the morphology and signal of leptomeningeal abnormalities. Because of the extra-axial hyperdensity seen on the CT, the patient was initially suspected to have subarachnoid hemorrhage. Cerebral CTA and DSA were subsequently normal, as were MRI and MRA of the spine. In addition, no causes of non-aneurysmal subarachnoid hemorrhage (such as reversible vasoconstriction syndrome) were seen. Due to further seizures, increased subarachnoid hemorrhage and unclear diagnosis, 6 weeks after presentation, brain biopsy was performed after multidisciplinary discussion.
In retrospect, the nodular nature of the leptomeningeal T1 hyperintensity in combination with the subarachnoid hemorrhage is concordant with the histological diagnosis, however the rarity of the condition made the diagnosis more difficult.
Further investigation with CT, FDG PET-CT, and clinical examination revealed no further disease. There was some uncertainty around whether this represented primary leptomeningeal melanomatosis or the much more common entity of meningeal disease secondary to metastatic melanoma, however the latter was considered more likely. Systemic treatment for melanoma was commenced but despite this, the patient unfortunately passed away 5 months after first presentation.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.