Presentation
Loss of appetite and abdominal discomfort.
Patient Data


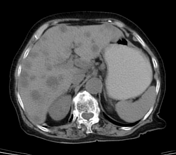

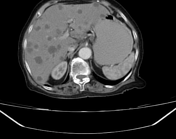

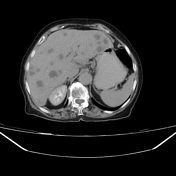



Multiple hypodense nodules are observed throughout the liver tissue, exhibiting peripheral enhancement in the early phases and washout in the delayed phase. This is consistent with hypovascular lesions, primarily possible from the gastrointestinal tract.
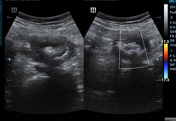
Normal liver parenchyma with no portal vein thrombosis. However, there is a short segmental thickening of the colonic wall (2 cm) at the hepatic flexure, with no complete obstruction. The proximal segment of the colon is not dilated, while the distal segment is not collapsed. Small-medium-sized hypo-attenuated lymph nodes are observed at the left para-aortic, near the left renal vessels, and at the pre-pancreatic area.
These findings are suggestive of colonic carcinoma with liver and lymph node metastasis.
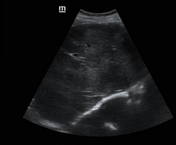

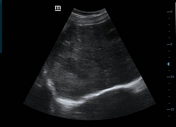

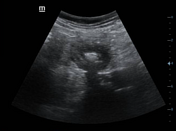



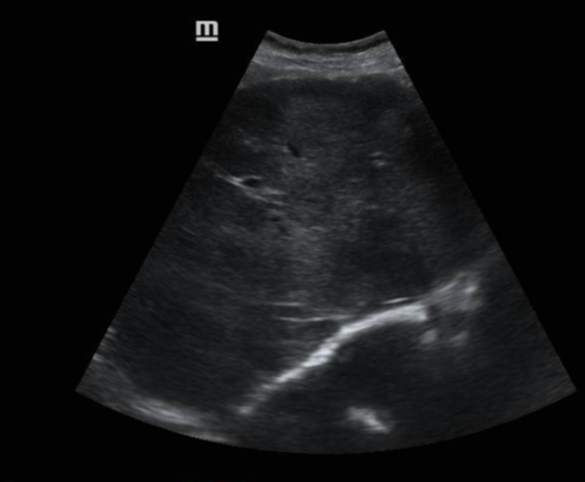
Ultrasound shows multiple small hypoechoic foci dispersed throughout the hepatic tissue, with the majority being hypoechoic and a few appearing hyperechoic. These ultrasound findings support the results obtained from the CT scan.
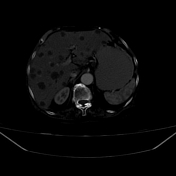
Segmental circumferential colonic wall thickness of hepatic flexure, biopsy needle in the wall of colon.
Case Discussion
Biopsies were taken from both the colon and the liver.
Histopathology results are shown below:
Gross: two small pieces from a Tru-Cut needle biopsy of a colonic mass labelled (1), and four pieces from liver deposits labelled (2); all pieces were submitted in total.
Microscopic examination:
1. colonic biopsy: showed colonic wall infiltrate by strips and clusters of atypical columnar cells with hyperchromatic nuclei and numerous signet ring cells, floating in lakes of extracellular mucin, surrounded by fibrous bands and reactive small lymphocytes
2. liver biopsy: showed hepatic tissue infiltrate by closely backed glands, strips and clusters of columnar cells with hyperchromasia, and numerous signet ring cells, floating in lakes of extracellular mucin
Conclusion: colonic mass: mucinous carcinoma with liver metastasis.
The most common sites of primary malignancy that metastasise to the liver are the gastrointestinal tract as in this case 1. Hypovascular hepatic metastases are usually from colon 'as in our case', lung, breast, and gastric carcinomas 2. Hepatic metastases may develop early enhancement with variable degrees of washout and peripheral rim enhancement.
Both ultrasound and CT scans can serve as viable alternatives to colonoscopy for examining symptomatic patients who may have colonic cancer. Utilising these methods could significantly decrease the reliance on colonoscopy in this group of patients, cost, time-saving 3, and an alternative choice.
Sometimes, in a limited resource setting, there is the absence of Immunohistochemistry and proper colonoscopy, which are capable of reaching the abnormal segment in the colon and taking deep enough samples with guaranteed results. A delayed diagnosis may lead to intestinal obstruction and emergency surgery later.
Take home message: giving sufficient time to examine the patient carefully, a complete diagnosis can be obtained.
This patient began treatment within couple days of the screening and intervention.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.