Presentation
4 weeks of headache. Behaviour change in the last few days. Bidirectional nystagmus. No seizures.
Patient Data
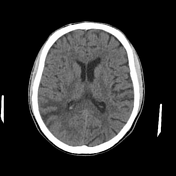







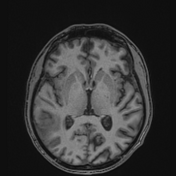
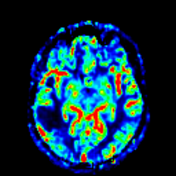
A region of hypodensity in the temporal and parietal lobes on the right primarily involves the white matter but, in some locations, appears to involve the cortex. No haemorrhage.
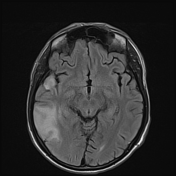

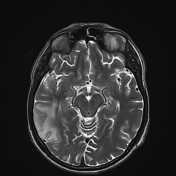



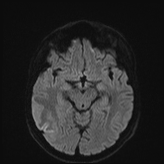

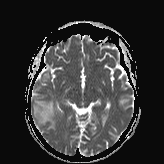

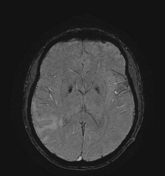




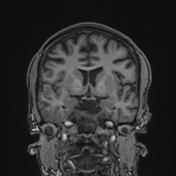

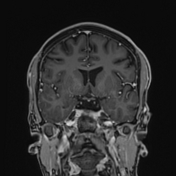

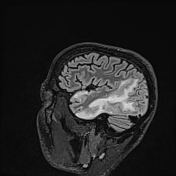

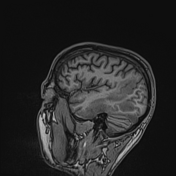

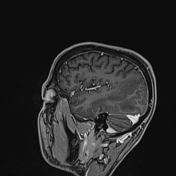

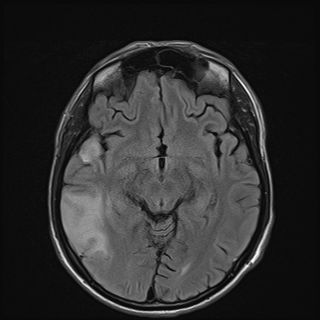
There is a diffuse FLAIR signal abnormality centred on the posterior aspect of the right temporal lobe extending into the occipital lobe and inferior parietal lobule. Further signal abnormality within the right anterior temporal pole, which is in continuity with the primary abnormality (best appreciated on sagittal). Signal abnormality involves both the cortex and subjacent white matter.
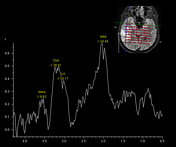
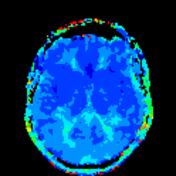
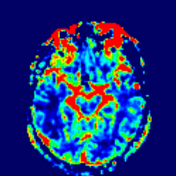
Despite the extent of abnormality, positive mass effect is minimal. Although the majority of the lesion shows facilitated diffusion (in the white matter), there is cortical preserved and possibly additional restricted diffusion in most of the affected cortex, especially inferiorly. CBV is reduced. MRS is non-contributory, with only minor elevation of choline in some areas. Small foci of susceptibility signal loss within the lesion.
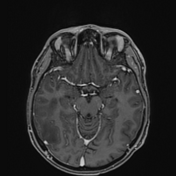
Prominent leptomeningeal enhancement along the inferior margins of the temporal lobe, particularly overlying the petrous temporal bone, without middle ear effusion or abnormal enhancement.
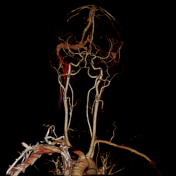
Cerebral veins and dural venous sinus appear normal. The remainder of the intracranial appearances is within normal limits.
Conclusion
Diffuse signal abnormality centred on the right temporal lobe with involvement of the parietal and occipital lobes demonstrating leptomeningeal enhancement at the inferior margins most likely represents an evolving/ resolving inflammatory/ischaemic process.
Possibilities, especially in this age group, include meningoencephalitis and myelin oligodendrocyte glycoprotein antibody-associated disease (MOGAD). Mitochondrial encephalomyopathy lactic acidosis and stroke-like episodes (MELAS) is another possibility.
In the absence of venous thrombosis or gyral cortical enhancement, a resolving venous infarct or ischaemic infarct is thought unlikely. A neoplasm is also considered very unlikely; certainly not typical astrocytoma/ glioblastoma. Occasionally, lymphoma can have an unusual presentation, especially if there is a history of immunosuppression.
Case Discussion
The patient went on to have blood DNA sequenced which confirmed the diagnosis of MELAS.
Report
The variant NC_012920.1:m.3243A>G, associated with MELAS, was detected. This variant is linked to the patient’s symptoms of headache, confusion, hearing loss, ophthalmoplegia, and ptosis. The heteroplasmic level in the blood DNA sample is about 48.2%, though this can vary across tissues.
Further analysis of urine DNA is recommended. Disease progression predictions based on heteroplasmic levels require adjustments for age and gender. The variant is maternally inherited.
Method
Sanger Sequencing using ABI BDT V3.1
QSV Analysis
PCR-RFLP (Polymerase Chain Reaction-Restriction Fragment Length Polymorphism)
Limit of detection: >3%




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.