Presentation
Typical angina. Elevated troponin T: 0.48 µg/L and C-reactive protein (CRP): 98 mg/L. History of previous respiratory tract infection.
Patient Data



















Findings:
Heart rate: 67 bpm, hematocrit: 0.38
Image quality: some respiratory artifacts, otherwise no limitations
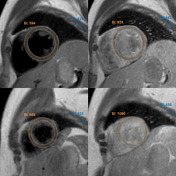
Morphology and functional analysis:
- LV-EDVI: 71 mL/m²
- LV-ESVI: 27 mL/m²
- LV-SVI: 43 mL/m²
- LV-EF: 61%
- cardiac output: 5.3 L/min
- cardiac index: 2.9 L/min/m²
- LV-ED wall + papillary mass: 99 g
- septum thickness: 10 mm
No regional left ventricular wall motion abnormalities.
Visually normal atrial size.
No significant cardiac valve pathology detected.
No intercavitary thrombi found.
Myocardial tissue properties (according to Lake Louise criteria II)1:
Regional myocardial edema in the apical segments best visible in the lateral wall.
Patchy intramyocardial and subepicardial late gadolinium enhancement (LGE) visible in the apical lateral and midventricular antero- and inferolateral segments.
T1 mapping: native T1 >1100 ms [948-1060 ms*], extracellular volume (ECV) 32-35%
* native T1 reference range based on local data
Minimal pericardial enhancement without thickening, adjacent to the left ventricular free wall.
No pericardial effusion.
Small bilateral pleural effusions.
Impression:
Cardiac MRI findings are consistent with acute inflammatory changes of the myocardium or acute myocarditis.


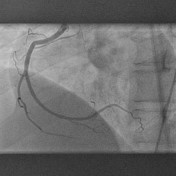


Coronary angiogram (on admission, 10 days prior to the MRI)
Normal left anterior descending (LAD), circumflex (Cx) and right coronary (RCA) arteries.
No evidence of stenosis or obstruction.
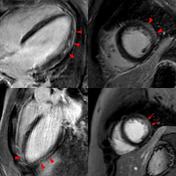

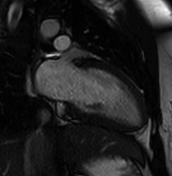
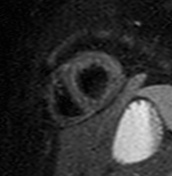
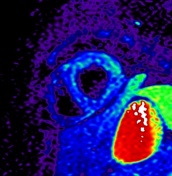
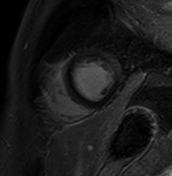
T2 black-blood / short tau inversion recovery (STIR) imaging:
Focal myocardial edema can be seen in the apical and mid free lateral wall on T2 black-blood images (blue arrowheads) and not so obvious in the STIR images (blue arrows). It can be visualized with a color map.
Myocardial edema can be also assessed by calculating the T2 signal intensity ratio between myocardium and skeletal muscle within the same image 1,2.
In this case, the T2 ratio was 2.3 - a T2 ratio of ≥2 is considered abnormal, provided images were acquired with the MRI integrated body coil (Q-body) 2-4.
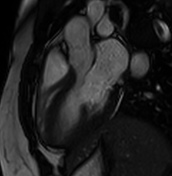
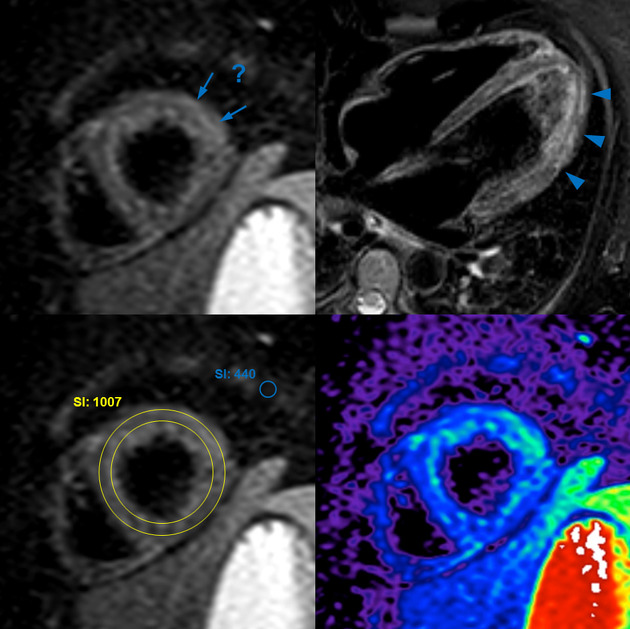
Early gadolinium enhancement:
Myocardial hyperemia/capillary leakage can be assessed in T1 black-blood SE images by calculating myocardial early gadolinium enhancement (EGE) ratio 2-4.
The enhancement ratio between myocardium and skeletal muscle, in this case, is ≥7 and absolute myocardial enhancement ≥60%. An enhancement ratio of ≥4 is considered and 45% is considered abnormal, again provided that images were acquired with the MRI integrated body coil (Q-body) 2-4.
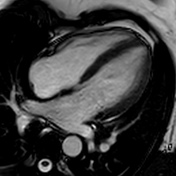
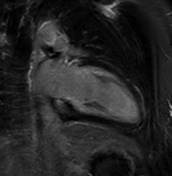
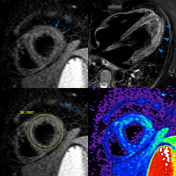
Late gadolinium enhancement (LGE):
Patchy intramyocardial and focal subepicardial late gadolinium enhancement can be seen on IR-GE images (red arrowheads) and on short-axis PSIR images (arrows), which is a characteristic pattern in myocarditis5 and reflects myocardial injury, but is neither a very sensitive nor specific feature if used exclusively1-5.
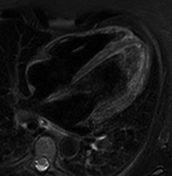
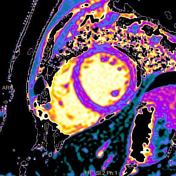
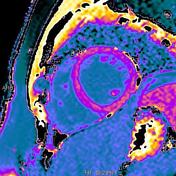
T1 mapping native and postcontrast:
Increased native T1 in the antero- and inferolateral midventricular segments is measured and displayed on a color-map T1 >1150 ms, z-score of >5 (based on local data).
The application of gadolinium leads to a shortening of T1 and even more so in the inflamed segments of the myocardium, which can be appreciated especially in the lateral wall.
Extracellular volume (ECV) was 32-35% in the antero- and inferolateral midventricular segments.
Case Discussion
This case illustrates MR imaging features of acute myocarditis and reviews the assessment according to the Lake Louise criteria 1,2.
Both main criteria are fulfilled following the updated new version 1:
- myocardial edema (based on T2w images or T2 mapping)
- non-ischemic myocardial injury (abnormal native T1, ECV or LGE)
There are no supportive criteria (pericarditis, systolic dysfunction) present.
Also, three out of three criteria (edema, EGE, LGE) of the old version 2 are met.
After the exclusion of coronary artery disease or recent childbirth and in the absence of any systemic disease as rheumatoid arthritis, systemic lupus erythematosus (SLE), or sarcoidosis, and in view of the supportive clinical findings, the diagnosis of myocarditis can be rated as certain.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.