Presentation
The patient initially presented to a local clinic with a long bone fracture that was not attributable to a low-velocity mechanism. Subsequent investigations revealed the onset of diabetes mellitus and hypertension. Further endocrinological evaluation by a specialist confirmed a diagnosis of Cushing syndrome, which necessitated bilateral adrenalectomies. Five years postoperatively, the patient developed progressive headaches and visual deterioration, prompting further medical evaluation.
Patient Data
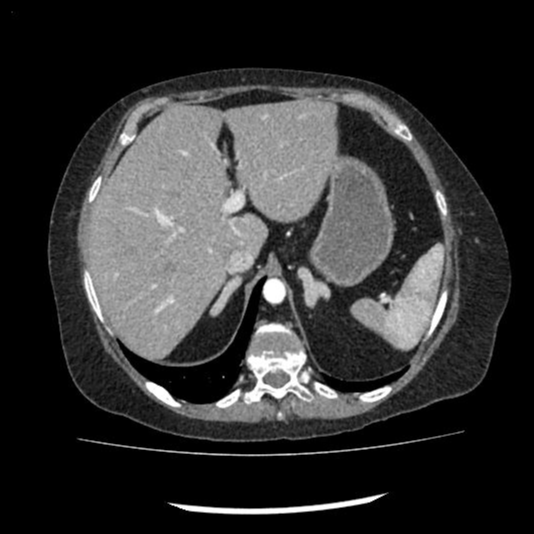
The axial abdominal CT image in the arterial phase demonstrates bilaterally symmetrical hypertrophied adrenal glands.


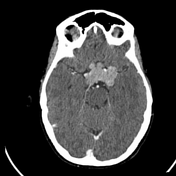


Axial brain CT images, both pre- and post-contrast, demonstrate a significant mass within the sellar and suprasellar regions, consistent with a pituitary macroadenoma. The mass is clearly visualised extending superiorly from the sella turcica, encroaching upon the suprasellar cistern. On post-contrast imaging, the lesion exhibits homogenous enhancement.
This mass effect is concerning for compression of adjacent structures, particularly the optic chiasm, which correlates clinically with the patient’s reported visual disturbances. This imaging pattern is characteristic of macroadenomas, which may arise secondary to conditions such as Cushing’s disease or other endocrine abnormalities.
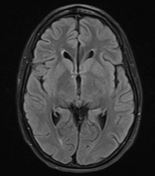

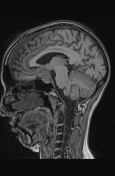

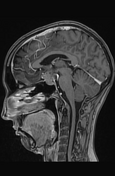

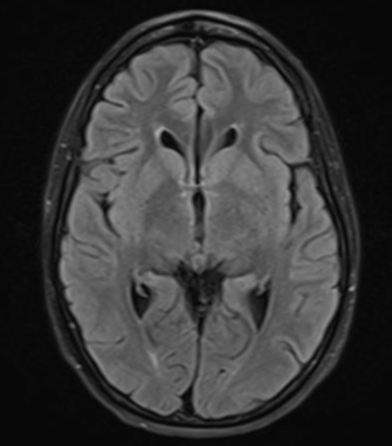
MRI reveals a microlobulated sellar-suprasellar lesion that is isointense to grey matter on both T1- and T2-weighted sequences, with moderate post-contrast enhancement.
Case Discussion
Patient presented with an unexplained long bone fracture, subsequently diagnosed with diabetes mellitus and hypertension. Further endocrinological evaluation revealed Cushings syndrome, necessitating bilateral adrenalectomies to manage the hypercortisolemia 1.
Following bilateral adrenalectomy for the management of Cushing syndrome, the patient developed a pituitary macroadenoma within five years, a condition known as Nelson syndrome. Nelson syndrome is a rare but recognised complication that occurs in individuals who have undergone adrenalectomy for Cushing’s disease. This condition is characterised by the rapid growth of an ACTH-secreting pituitary adenoma after the removal of the adrenal glands, due to the loss of feedback inhibition from cortisol 2.
In the absence of cortisol production, the pituitary gland continues to produce large amounts of ACTH, which can stimulate the enlargement of pre-existing pituitary adenomas or lead to the development of new ones. Clinically, Nelson syndrome presents with symptoms such as progressive headaches, visual disturbances, and hyperpigmentation due to excessive ACTH levels. The visual symptoms typically result from the mass effect of the macroadenoma on the optic chiasm.
In this case, the patient developed significant headaches and visual field defects, prompting surgical intervention to remove the tumour. However, when surgery failed to adequately control the tumour growth, radiation therapy was initiated as part of the management strategy for Nelson syndrome. This case underscores the importance of long-term monitoring in patients who undergo adrenalectomy for Cushing’s disease, as they remain at risk for this challenging postoperative complication.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.