Portal vein embolization
Updates to Case Attributes
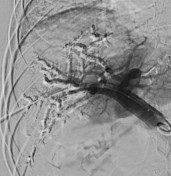
Portal vein embolization (PVE) is a technique used by interventional radiologists to improve the postoperative outcome of a hepatectomy.
When a part of the liver is resected, the remaining component is referred to as the future liver remnant (FLR). If this remnant liver were too small to supply the patient's body size, then the postoperative prognosis would be poor. PVE can "grow" the FLR by preoperatively occluding the lobe to be resected (almost always the right lobe). Increased blood flow to the left hepatic lobe, and serum factors released by the injured occluded liver, induce hyperplasia in the left hepatic lobe.
PVE is a relatively safe procedure, with postprocedure mortality reported at 0% and morbidity at 2.2% 1.
Portal hypertension is a major contraindication to PVE, since it will drive up portal pressures even further, possibly resulting variceal haemorrhage.
-<p><a title="Portal vein embolization" href="/articles/portal-vein-embolization">Portal vein embolization (PVE)</a> is a technique used by interventional radiologists to improve the postoperative outcome of a hepatectomy.</p><p>When a part of the liver is resected, the remaining component is referred to as the <a title="future liver remnant (FLR)" href="/articles/future-liver-remnant-flr">future liver remnant (FLR)</a>. If this remnant liver were too small to supply the patient's body size, then the postoperative prognosis would be poor. PVE can "grow" the FLR by preoperatively occluding the lobe to be resected (almost always the right lobe). Increased blood flow to the left hepatic lobe, and serum factors released by the injured occluded liver, induce hyperplasia in the left hepatic lobe.</p><p>PVE is a relatively safe procedure, with postprocedure mortality reported at 0% and morbidity at 2.2% <sup>1</sup>.</p><p><a title="Portal hypertension" href="/articles/portal-hypertension">Portal hypertension</a> is a major contraindication to PVE, since it will drive up portal pressures even further, possibly resulting variceal haemorrhage.</p>- +<p><a href="/articles/portal-vein-embolization">Portal vein embolization (PVE)</a> is a technique used by interventional radiologists to improve the postoperative outcome of a hepatectomy.</p><p>When a part of the liver is resected, the remaining component is referred to as the <a title="future liver remnant" href="/articles/future-liver-remnant">future liver remnant (FLR)</a>. If this remnant liver were too small to supply the patient's body size, then the postoperative prognosis would be poor. PVE can "grow" the FLR by preoperatively occluding the lobe to be resected (almost always the right lobe). Increased blood flow to the left hepatic lobe, and serum factors released by the injured occluded liver, induce hyperplasia in the left hepatic lobe.</p><p>PVE is a relatively safe procedure, with postprocedure mortality reported at 0% and morbidity at 2.2% <sup>1</sup>.</p><p><a href="/articles/portal-hypertension">Portal hypertension</a> is a major contraindication to PVE, since it will drive up portal pressures even further, possibly resulting variceal haemorrhage.</p>
Updates to Study Attributes
Image DSA (angiography) (Portal vein) ( update )