Presentation
Two weeks of progressive jaundice, nausea, vomiting, and generalised abdominal pain
Patient Data


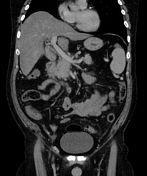



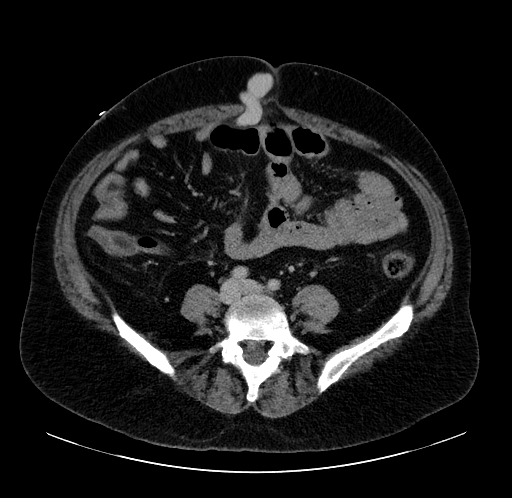
Heterogeneous liver parenchyma with nodular contour. No intra or extra-hepatic biliary duct dilatation. The portal and hepatic veins are patent. Normal appearance of kidneys, adrenals, and small and large bowel.
There is marked splenomegaly and splenic varices (axial, coronal, sagittal). Oesophageal, gastric, and rectal varices are also present. The IVC appears dilated.
A prominent recanalised paraumbilical vein runs inferiorly from the portal vein to the umbilicus. It continues within the rectus sheath inferiorly toward the pelvis where it joins the right external iliac vein.
Bulky head of pancreas and mild adjacent fat stranding raises the possibility of pancreatitis. Normal appearance of the pancreatic duct.
The thin-walled gallbladder is distended with intermediate to high density material of unclear significance. No pericholecystic fluid or fat stranding.
Well-defined area of low-attenuation within the hepatic parenchyma adjacent to the gallbladder likely represents focal fat.
These findings are in keeping with portal hypertension secondary to cirrhosis. There are no features of biliary obstruction.
Case Discussion
This is a 40-year-old male with a history of chronic alcohol excess. He was treated initially for presumed abdominal sepsis secondary to ascending cholangitis.
CT of abdomen and pelvis revealed no biliary tree obstruction but demonstrated features of cirrhosis and severe portal hypertension. The patient had no prior history of liver disease.
He was diagnosed with acute decompensated liver failure, with florid encephalopathy and profound jaundice with a serum bilirubin of nearly 600 µmol/L. The patient did not meet biochemical criteria for acute pancreatitis despite his alcohol history and the bulky appearance of the head of pancreas.
Chronic portal hypertension, usually secondary to cirrhosis, causes a backflow of pressure to areas of portosystemic anastomosis. This leads to the development of varices. The mortality associated with intra-abdominal varices is high, with roughly 33% lifetime mortality due to haemorrhage from either the oesophagus or stomach 1. This is complicated by inherent coagulopathy due to decreased synthetic function of the cirrhotic liver.
Focal hepatic steatosis can also be linked to portal hypertension. Delivery of blood by sources other than the portal vein or hepatic artery, such as an enlarged paraumbilical vein, can alter the haemodynamics of the liver parenchyma, leading to steatosis 2. This is referred to as the 'third inflow' effect.
This case demonstrates a spectrum of radiological findings of chronic liver disease and portal hypertension.
Case courtesy of Dr Phil Lewis.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.