Presentation
Haemodynamically-unstable with HR 105, BP 115/70 and haemoglobin drop from 140 (baseline) to 77. Worsening renal function, eGFR 58, usually >90. No history of trauma.
Patient Data


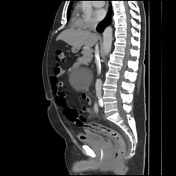

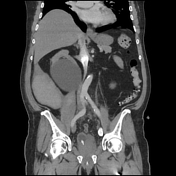

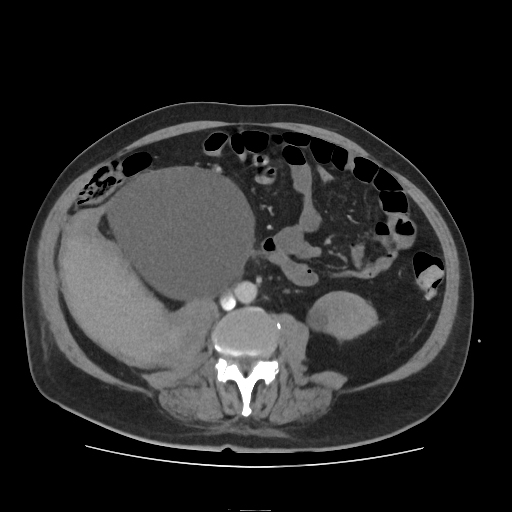
6.5 x 16.5 x 25.5 cm (ML x AP x CC) right-sided heterogeneous hyperdense retroperitoneal collection extending from the iliopsoas muscle to the lateral abdominal wall. No active extravasation of contrast medium seen on this portal venous study. No free gas.
Non-obstructed kidneys with cysts, largest in the mid right kidney is 13 cm.
1.3 cm hypodensity in hepatic segment 8 is indeterminate on a single phase study, most likely represents a benign cyst.
Otherwise solid abdominal viscera are unremarkable.
Large and small bowels are unremarkable.
Unremarkable abdominal aorta and its main branches.
Subtle low density filling defects of the segmental and subsegmental branches of the lower lobe pulmonary arteries bilaterally.
Urinary catheter noted. Prostatomegaly.
Conclusion:
1. Large right-sided acute retroperitoneal haematoma with no evidence of active bleeding
2. Pulmonary thromboses in situ and/or emboli (lung windows: not shown, demonstrate evidence of COVID-19 pneumonia)
Case Discussion
Spontaneous retroperitoneal haemorrhage is rare. Image-guided embolisation of supplying vessels is now deemed to be best practice, and therefore CT angiography is advised if not already done.
In this case, a follow-up CT angiography was performed 4 hours later and it did not show any evidence of active bleeding.
COVID-19 has a clear prothrombotic tendency. It was noted early in the pandemic that there was an increased prevalence of pulmonary thromboemboli in COVID-19.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.