Presentation
Football player presents with knee instability.
Patient Data


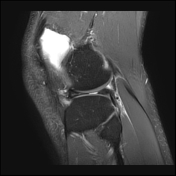

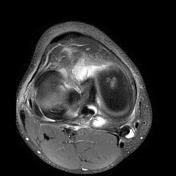






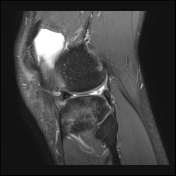
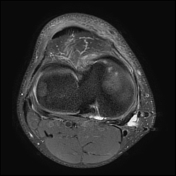
Radial tear of the lateral meniscal body, with displaced fragment folded back along the posterior horn.
Hyaline cartilage in the lateral compartment is intact; no subchondral marrow signal abnormality.
Focal chondropathy and subchondral marrow hyperintensity in the medial compartment anteriorly.
The patient had a partial lateral meniscectomy 1 month after initial MRI and represents with lateral knee pain 3 months post-arthroscopy.




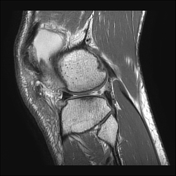



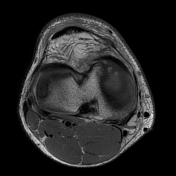


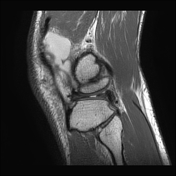
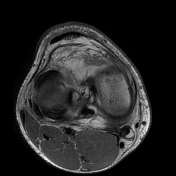
Debridement of the lateral meniscal tear with residual defect. Meniscal body remnant is extruded and macerated in the collateral gutter.
Interval partial-thickness chondral delamination over the lateral femoral condyle and lateral tibial plateau.
Subchondral insufficiency fracture has developed along the margin of the lateral tibial plateau, with associated reactive marrow hyperintensity. Minor depression of the articular surface is best appreciated on the coronal PD fs sequence.
Case Discussion
The meniscus is an extremely important structure in weight-bearing at the knee. Following arthroscopic debridement, altered load distribution and recurrent impaction result in progressive chondral damage and accelerated osteoarthrosis in the longer term.
Post-meniscectomy insufficiency fracture and osteonecrosis have also been described. Although the exact pathophysiology is unclear, these may be related entities. A combination of disuse osteopenia and increased focal contact pressures can result in a subchondral insufficiency fracture, with the ensuing bleeding and bone "oedema" causing vascular insufficiency and thus osteonecrosis.
Conversely, vascular insufficiency could be the primary cause of osteonecrosis, with subsequent trabecular failure and fracture.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.