Presentation
Persistent and recurrent vomiting for months with electrolyte imbalance (hypocalcemia).
Patient Data
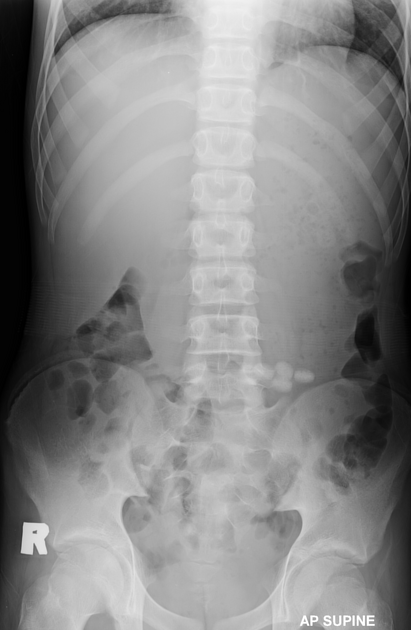
Grossly distended stomach with food particles and fluid filled.
No small bowel or large bowel loops dilatation.
No pneumoperitoneum.







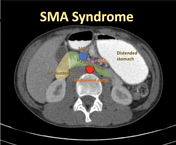
Marked dilatation of the stomach, first (D1), second (D2) and proximal third (D3) parts of duodenum with transition point at the aortomesenteric region (between the superior mesenteric artery (SMA) and abdominal aorta). These proximal bowel loops dilatation were filled with positive oral contrast. Relatively lack of fat surrounding SMA. The D3 duodenum at the aortomesenteric region has significant reduced in caliber and appeared to be compressed by the SMA and abdominal aorta. The distal bowel loops are normal in caliber and the positive oral contrast can flow through this compression.
No pneumoperitoneum or ascites.
The aortomesenteric angle and distance (measured at sagittal view of abdominal aorta) are 15 degrees and 7mm, which are abnormal values.
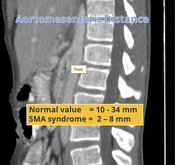
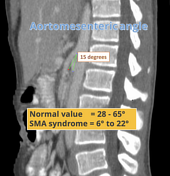

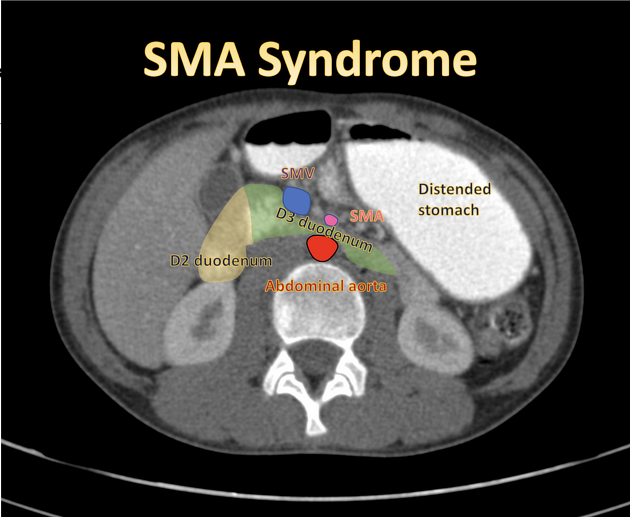
Annotated images for anatomy and radiological measurement related to superior mesenteric artery syndrome.
Case Discussion
Based on the radiological measurement of aortomesenteric angle and aortomesenteric distance between the superior mesenteric artery and abdominal aorta, in addition to the electrolyte imbalance and clinical history of persistent vomiting, the diagnosis of superior mesenteric artery syndrome was made.
SMA syndrome is a rare acquired vascular compression disorder in which acute angulation of the superior mesenteric artery (SMA) results in compression of the third part of the duodenum, leading to proximal bowel loops obstruction.
Patient was treated with parenteral nutrition and supplements initially. He gained weight with reduction of the vomiting symptoms as well as improvement of the electrolyte imbalance in clinic follow up.
Compression of the left renal vein at this region is being named as nutcracker syndrome.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.