Acute lymphoblastic leukaemia (ALL) is a malignant disorder of the bone marrow characterised by the proliferation of the lymphoid progenitor cells, typically of the B cell lineage.
On this page:
Epidemiology
Acute lymphoblastic leukaemia is the most common form of childhood leukaemia, accounting for ~80% of paediatric leukaemia cases 1. In adults, ALL corresponds to ~20% of leukaemia cases 1. Peak age is between 3 and 7 years, with a second peak over 40 years.
Clinical presentation
The clinical features of acute lymphoblastic leukaemia are non-specific. Children commonly have at least one pallor, fever, a palpable liver, a palpable spleen, or bruising on diagnosis 2. Other symptoms such as bone or joint pain, weight loss, anorexia, bleeding, abdominal pain and abdominal distension are also common.
Pathology
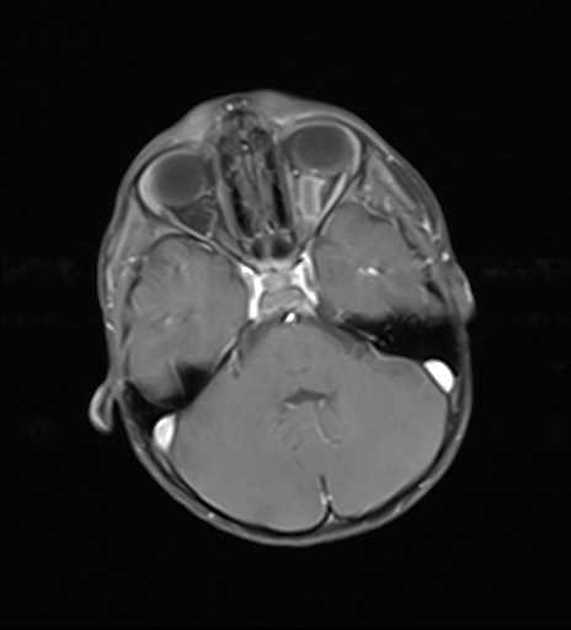
In acute lymphoblastic leukaemia, the lymphoid progenitor cells, also known as lymphoblasts, do not mature due to abnormal expression of genes, often as a result of chromosomal abnormalities or chromosomal translocations (e.g. BCR-ABL1). The proliferation of the primitive cells takes up more and more marrow space at the expense of the normal haematopoietic elements, resulting in a decrease in the production of normal blood cells and bone marrow failure. Eventually, the lymphoblasts spill into the blood and can affect the liver, spleen, central nervous system, and lymph nodes.
Radiographic features
Plain radiograph
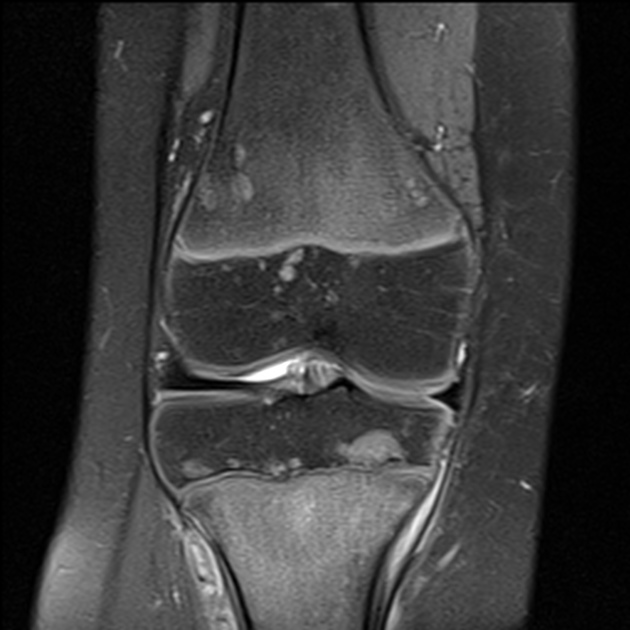
Bone lesions are common in leukaemia. A metaphyseal radiolucent band is one of the most important radiological findings 3. Other radiological findings include subperiosteal new bone formation and osteolytic lesions involving the medullary cavity and cortex 1,3-5.
Chest radiographs may reveal a mediastinal mass.
Treatment and prognosis
The treatment for acute lymphoblastic leukaemia typically has three phases:
induction therapy: combination chemotherapy is used to rapidly kill tumour cells to get the patient into remission
consolidation phase: if remission is achieved, further chemotherapy is given during this phase to treat the residual disease
-
maintenance phase: if the patient is still in remission after the consolidation phase, maintenance oral therapy is given
this may last up to three years if the patient remains in remission
The exact treatment regimens used in managing ALL are beyond the scope of this article, but depend on factors such as whether the disease is B or T cell ALL, and whether positive or negative for BCR-ABL1 fusion.
Paediatric patients with acute lymphoblastic leukaemia have an overall five-year survival rate of 80% depending on their risk profile 6. However, only 30-40% of adults with ALL achieve long-term remission with the treatment regimens 7.
Differential diagnosis
For acute lymphoblastic leukaemia bony abnormalities, consider:






 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.