Allergic bronchopulmonary aspergillosis (ABPA) is at the mild end of the spectrum of disease caused by pulmonary aspergillosis and can be classified as an eosinophilic lung disease 2-4.
On this page:
Epidemiology
This entity is most commonly encountered in patients with longstanding asthma, and only occasionally in patients with cystic fibrosis 4,5. Only rarely does it appear in patients with no other identifiable pulmonary illness 5.
In general, patients are young and are diagnosed before the age of 40 years 9.
It is considered the most common cause of eosinophilic lung disease in developed countries 13.
Clinical presentation
Clinically, patients have atopic symptoms (especially asthma) and present with recurrent chest infections. They may expectorate orange-coloured mucous plugs.
A clinical staging system has been developed 9:
stage I: acute
stage II: remission
stage III: recurrent exacerbation
stage IV: steroid-dependent asthma
stage V: pulmonary fibrosis
Major and minor criteria have also been established 5,6.
-
major criteria
-
clinical
asthma (approximately 90% of patient may have asthma 14)
-
radiographic features
pulmonary opacities (transient or chronic)
central bronchiectasis
-
immune system
blood eosinophilia
immediate skin reactivity to Aspergillus antigen (elevated IgG and/or IgE against A. fumigatus)
increased serum IgE (>1000 IU/ml)
-
-
minor criteria
fungal elements in sputum
expectoration of brown plugs/flecks
delayed skin reactivity to fungal antigens
ASPER criteria include asthma/atopy history, serum IgG or IgE against Aspergillus spp., proximal (central) bronchiectasis, IgE levels >1000ng/mL, and reactive skin test.
Pathology
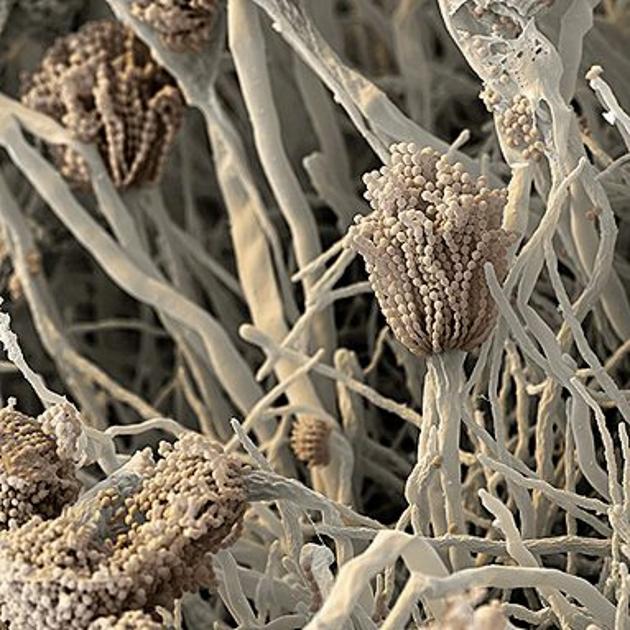
Allergic bronchopulmonary aspergillosis is the result of hypersensitivity towards Aspergillus spp (esp fumigatus) which grows within the lumen of the bronchi, without invasion. The hypersensitivity initially causes bronchospasm and bronchial wall oedema, which is IgE-mediated. Ultimately, there is bronchial wall damage with loss of muscle and bronchial wall cartilage resulting in bronchiectasis (typically central bronchiectasis) 7. Both types I and III allergic reactions have been implicated 4.
Bronchocentric granulomatosis often occurs, which is characterised by necrotising granulomatous inflammation that destroys the walls of small bronchi and bronchioles. Macroscopically, the mucous plugs are orange/brown in colour.
Segmental and subsegmental bronchi are dilated and filled with mucus, admixed with eosinophils and occasional fungal hyphae 4,7. Charcot-Leyden crystals may be prominent 7.
Markers
Laboratory findings include:
elevated Aspergillus-specific IgE
elevated precipitating IgG against Aspergillus
peripheral eosinophilia
positive skin test
Radiographic features
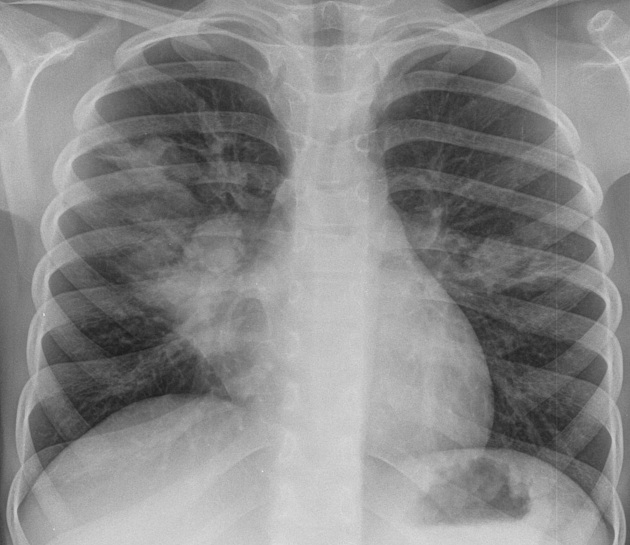
Plain radiograph
Early in the disease chest x-rays will appear normal, or only demonstrate changes of asthma. Transient patchy areas of consolidation may be evident representing eosinophilic pneumonia.
Eventually, bronchiectasis may be evident. Mucoid impaction in dilated bronchi can appear mass-like or sausage-shaped or branching opacities (finger in glove sign). Pulmonary collapse may be seen as a consequence of endobronchial mucoid impaction.
Fleeting shadows over time can also be a characteristic feature of this disease 14. These opacities usually appear and disappear in different areas of the lung over a period of time as transient pulmonary infiltrates.
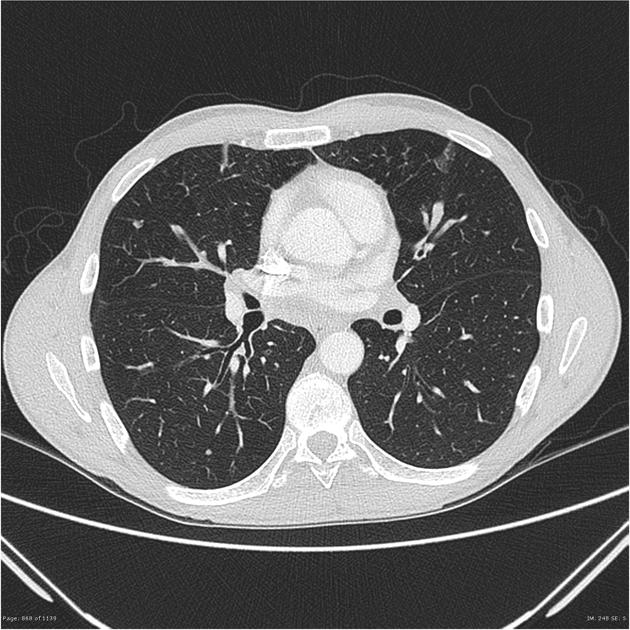
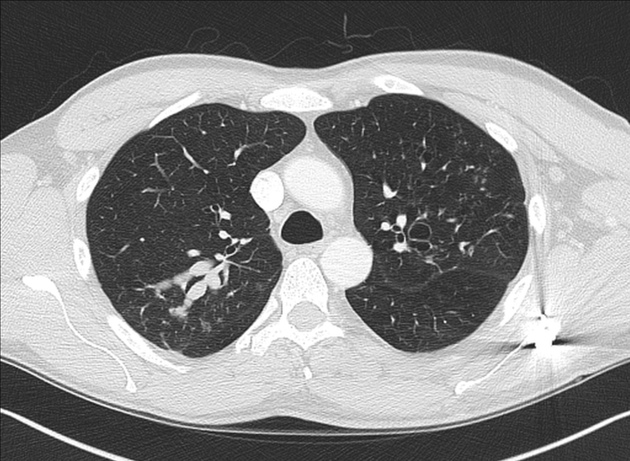
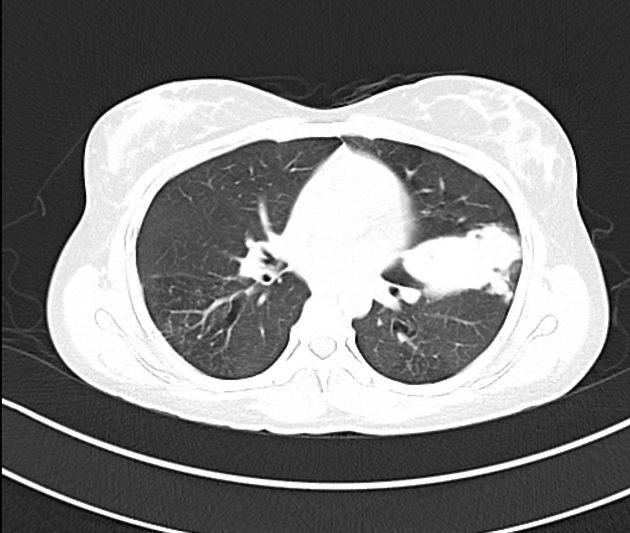
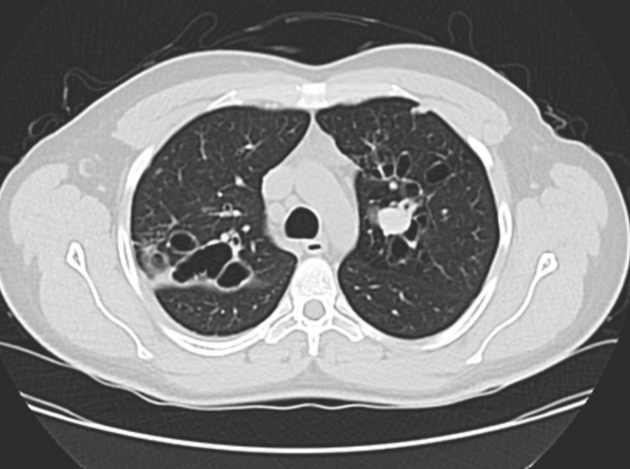
CT
CT findings include:
fleeting pulmonary alveolar opacities: common
centrilobular nodules representing dilated and opacified bronchioles 4
-
central, upper lobe saccular bronchiectasis involving segmental and subsegmental bronchi is characteristic
mucoid impaction results in a bronchocoele, the finger in glove sign
this may give a Y, V or toothpaste-like configuration
centrilobular nodular opacities.
high attenuation mucus +/- (calcification) in impacted mucus in ~30% 3,4
bronchial wall thickening: common
chronic disease may progress to pulmonary fibrosis, predominantly in the upper lobe
cavitation: 10%
Treatment and prognosis
Treatment of allergic bronchopulmonary aspergillosis is difficult due to the ubiquity of Aspergillus in the environment. The main focus of treatment revolves around 8:
managing asthma
limiting/controlling exacerbations: corticosteroid plays a major role
eradicating Aspergillus from the airway: antifungal agents, e.g. ketoconazole
preventing late complications, e.g. severe bronchiectasis, fibrosis
Many patients are successfully managed after diagnosis and never progress clinically to stage IV or V. In stages I to III, prognosis is excellent, whereas stage V has high 5-year mortality from respiratory failure 9.
History and etymology
ABPA was first described by K F W Hinson et al in 1952 15
Differential diagnosis
For a discussion of the differential diagnosis of bronchiectasis please refer to the article bronchiectasis and more specifically central bronchiectasis.
For mucoid impaction consider:
mucoid impaction secondary to bronchiectasis
secondary to an endobronchial lesion
secondary to atretic bronchial segment








 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.