Blunt cerebrovascular injury (BCVI), sometimes called blunt cervicovascular injury or blunt carotid and vertebral artery injury, refers to a spectrum of uncommon but potentially devastating injuries to the intracranial and extracranial carotid and vertebral arteries due to blunt trauma.
On this page:
Epidemiology
Blunt cerebrovascular injury is often part of multitrauma with a significant series of blunt trauma CTA reporting an incidence of approximately 1% 3. A large systematic review and meta-analysis of more than 120,000 trauma patients reported an incidence ranging from 0.18 to 2.7% 7.
Pathology
Primarily, blunt cerebrovascular injury is caused by longitudinal stretching 1 and/or crush injury to the vessels.
stretch injury: acceleration-deceleration can cause rotation, distraction, and hyperextension of the neck, stressing the craniocervical vessels, which is the mechanism for the most common cause of BCVI: motor vehicle collisions
crush injury: less common whereby a direct blow to the neck or base of the skull may cause a crush injury to the carotid or vertebral arteries; other causes for crush injury include compression from fracture fragments from the carotid canal or cervical spine, or between fractured structures
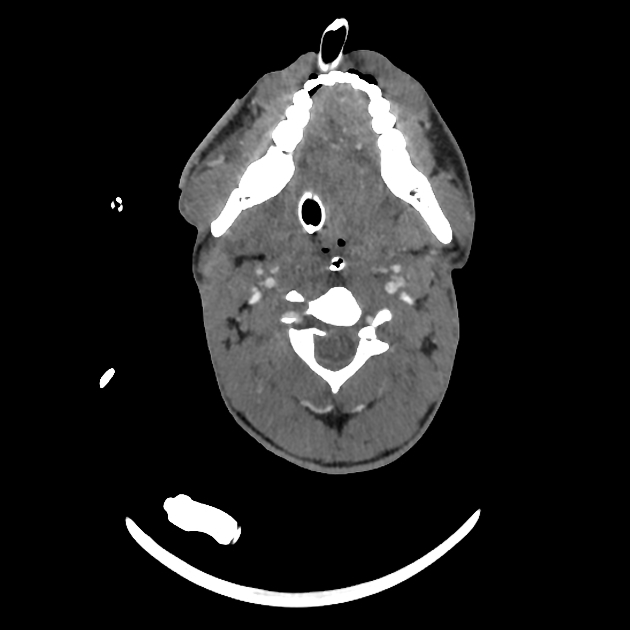
Blunt cerebrovascular injury can affect multiple vessels (18-38%) and occurs in typical locations where there is relative fixation 1:
-
cervical ICA just below the skull base
petrous ICA
cavernous ICA (entry to and exit from the cavernous sinus where dural attachments exist)
-
origin
bifurcation
-
origin
cervical vertebral artery as it passes through the transverse foramina
as it pierces the dura at the foramen magnum
Screening
Several screening tools have been developed to identify those at risk of blunt cerebrovascular injury and limit the use of angiography:
Denver criteria 6: subsequently modified and refined, is the most widely used and validated criteria 11
In general, BCVI is at higher risk if there is a high energy transfer mechanism along with clinical or imaging evidence of significant craniofacial, cervical, or upper thoracic injuries. About 70% are associated with cervical spine fractures 8.
Classification
The Biffl scale 2 describes the vascular injury on angiography (either CTA or DSA) on a scale of I to V, with higher grades of carotid injury associated with a high risk of stroke.
Radiographic features
CT
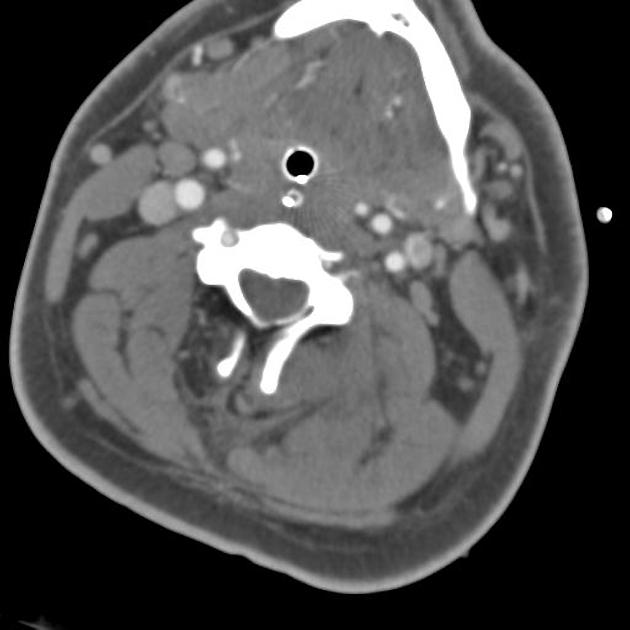
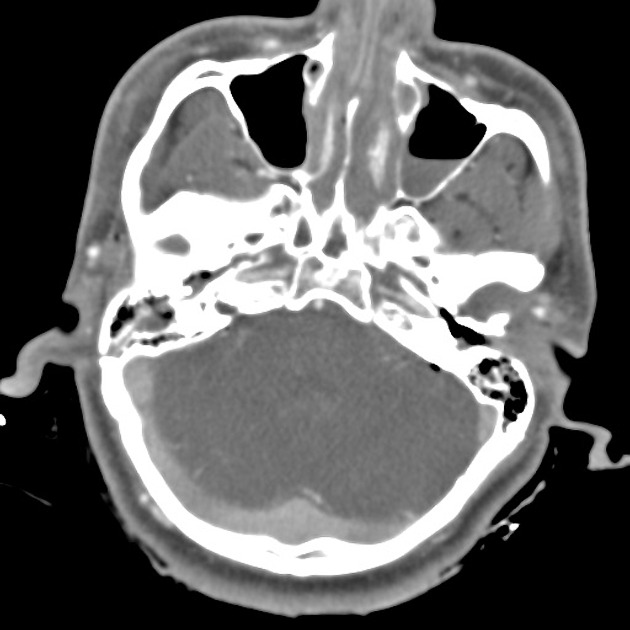
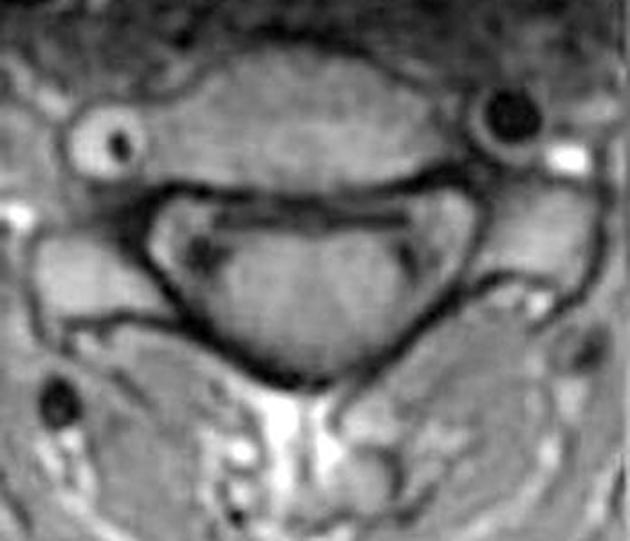
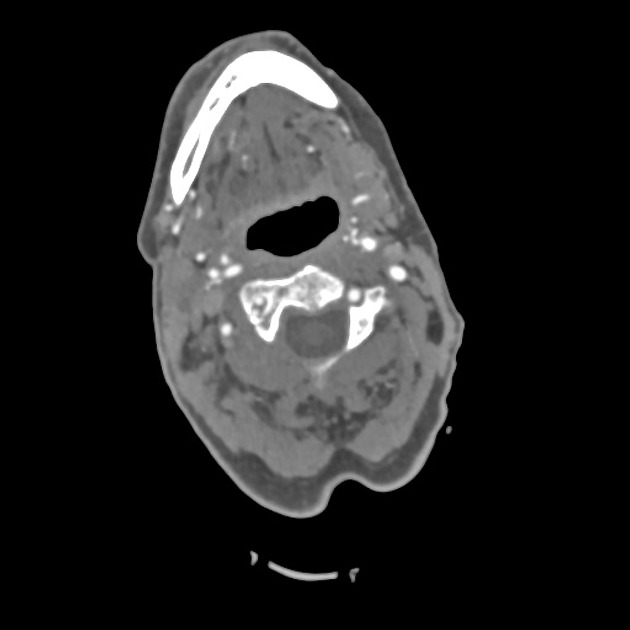
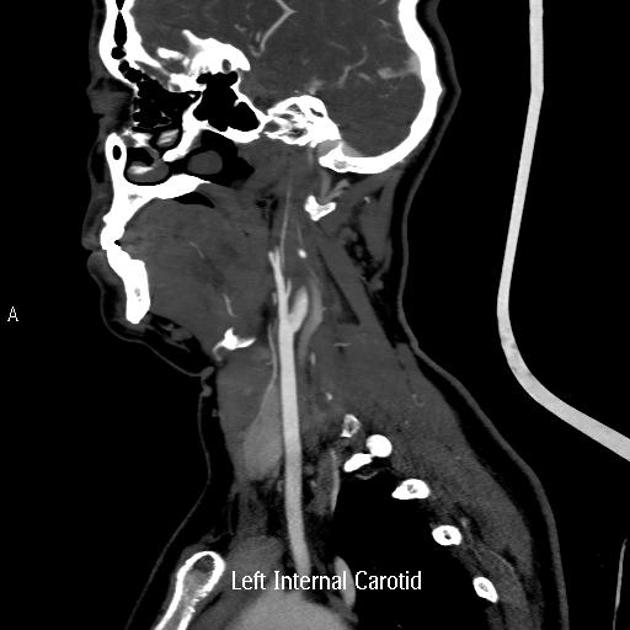
Signs on CT angiography of blunt cerebrovascular injury include 1
minimal intimal injury (irregularity)
intimal flap
dissection with or without intramural haematoma
transection
vessel occlusion
AV fistula
Angiography (DSA)
The signs of blunt cerebrovascular injury on digital subtraction angiography (DSA) are the same as CTA. A 2011 study of screening 32-channel multidetector CT compared to DSA showed that DSA is far more sensitive than CTA 4.
Treatment and prognosis
When undiagnosed, blunt cerebrovascular injury has high morbidity and mortality, primarily from cerebral infarction. A significant minority of patients will have an asymptomatic interval - which could be hours to months. The majority of infarcts occur within 72 hours, with the peak incidence of symptoms being 13-24 hours - thus, there is a potential therapeutic window to treat these patients whilst they are asymptomatic.
The risk for stroke with carotid injury depends on the grade of injury (see separate article on Biffl grade). The risk of cerebral infarction following BCVI is reduced with antithrombotic/antiplatelet therapy, but this can be a difficult management decision as often there is also concomitant intracranial haemorrhage from the primary trauma. In select cases, stenting of the injured vessel or open surgical repair is performed.
Differential diagnosis
technical and patient artifacts
anatomic vascular variants







 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.