Bowel obstructions are common and account for 20% of admissions with "surgical abdomens". Radiology is important in confirming the diagnosis and identifying the underlying cause.
Bowel obstructions are usually divided according to where the obstruction occurs, and since imaging appearances, underlying pathology, and treatment differ, these are discussed separately:
Bowel obstruction may be complete or incomplete. Complete or high grade obstruction means that no fluid or gas can go beyond the obstruction. Incomplete, low grade or partial obstruction means that fluid or gas are still able to get past 6.
On this page:
Clinical presentation
The classic clinical features of bowel obstruction are:
colicky abdominal pain
vomiting
abdominal distension
absolute constipation
unstable vital signs
acidotic blood gas as seen in bowel ischaemia 3
The order and timescale in which these appear to vary depending on whether there is large or small bowel obstruction. Absolute constipation and pain are more prominent early on in large bowel obstruction while vomiting is the predominant early feature for small bowel obstruction 3.
Additional features are dependent on the exact underlying pathology.
Pathology
Aetiology
Small bowel obstruction
adhesions
Large bowel obstruction
volvulus
Radiographic features
Imaging plays an important role in both diagnosing bowel obstruction as well as helping determine the choice and timing of appropriate management. The main aims of imaging in cases of suspected bowel obstruction are:
differentiate true mechanical obstruction from ileus or constipation
localise the site of obstruction
identify an underlying cause
assess for complications (e.g. ischaemia or perforation)
assess the viability of bowel segments involved
Plain radiograph
Plain abdominal radiographs are used as a screening tool for bowel obstruction but do not exclude this if they are normal. The main findings include dilated bowel loops (see 3-6-9 rule) with or without the presence of fluid levels. Erect chest radiographs can also be used to screen for complicating perforation.
In paediatrics, bowel is considered dilated when the normal honeycomb/polygonal appearances of the bowel is lost 4. Besides, if the diameter of the bowel is more than the transverse diameter of the vertebrae 4 (more specifically interpedicular width of the L2 vertebrae) the bowel is also considered as dilated 5.
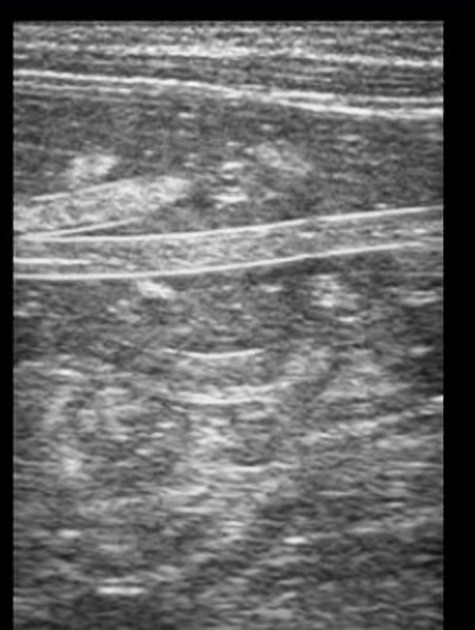
Ultrasound
Dilated small bowel loops greater than 2.5 cm in diameter is suggestive of small bowel obstruction. Ultrasound has 90% sensitivity and 96% specificity in diagnosing small bowel obstruction 3.
Identifying that large bowel obstruction is present is as good as CT. However, CT scan is better at finding the cause of the obstruction 3.
CT
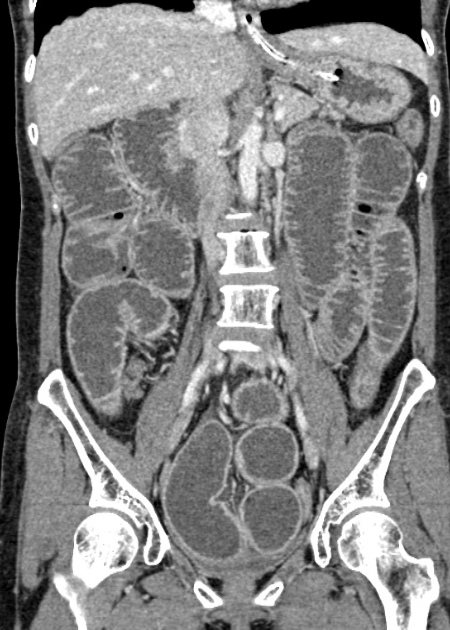
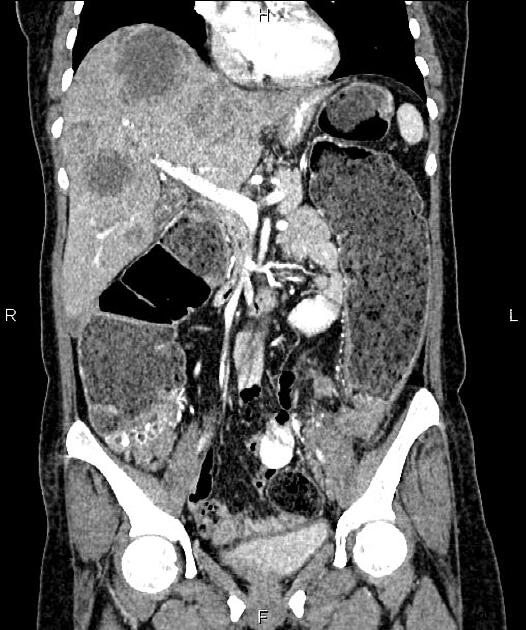
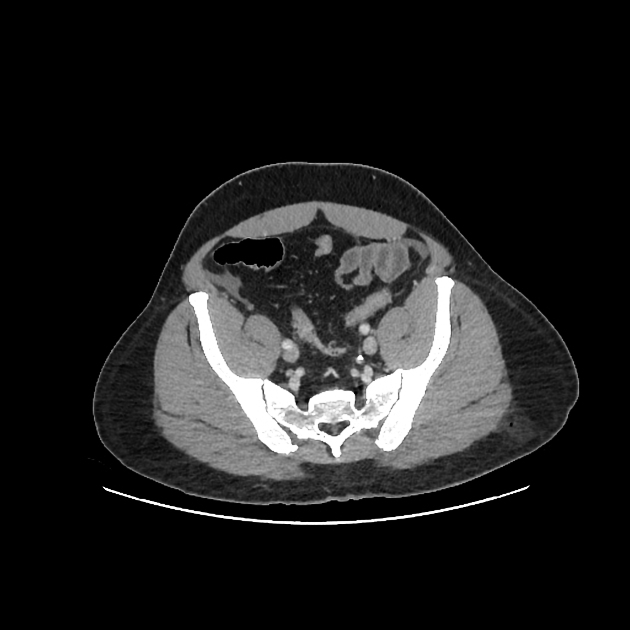
Plain radiographs are increasingly being replaced by CT to assess for bowel obstruction. Although the precise findings vary with the underlying pathology and localisation of the obstruction, common findings include:
a distinct transition point where bowel calibre changes from normal to abnormal
-
dilated bowel loops proximal to the transition point
small bowel >3.0 cm
large bowel >5 cm
a small bowel size threshold of 2.5 cm increases sensitivity for partial small bowel obstruction
collapsed or normal calibre bowel distal to the transitional point
bowel wall thickening
surrounding mesenteric fat stranding indicating inflammation
twisting of the mesentery in cases of volvulus
If bowel obstruction is identified it is important to assess for complications and assess the viability of the involved bowel:
pneumoperitoneum indicating perforation
-
as for ischaemia but for bowel within a hernial sac
Treatment and prognosis
Once intestinal obstruction is confirmed imaging findings can guide the timing of any planned surgical intervention. In cases where there are signs of ischaemia (i.e. strangulated bowel obstruction), emergency surgery may be needed to salvage bowel. The presence of frank perforation and peritonitis will need surgical washout.
The extent of involved bowel may determine whether or not a laparoscopic approach can be employed as well as help guide the size of the opening surgical incision.









 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.