Calcified cerebral embolus is an uncommon and often overlooked cause of embolic ischaemic stroke.
On this page:
Epidemiology
Although emboli are a common cause of ischaemic stroke, calcified cerebral emboli are considered rare. With only a paucity of literature regarding calcified cerebral emboli (only 48 reported cases as of 2014) it is difficult to truly gauge the incidence of stroke via this aetiology 1. However, one relatively large 2014 study found that calcified cerebral emboli were detected in 3% of all patients undergoing non-contrast CT with the clinical indication of stroke, many of these cases only detected retrospectively during the study 1.
Clinical presentation
The presentation is that of acute ischaemic stroke, which is discussed in more detail elsewhere (see ischaemic stroke) 1-3. However, these emboli may also be found incidentally without prior evidence of stroke 1.
Pathology
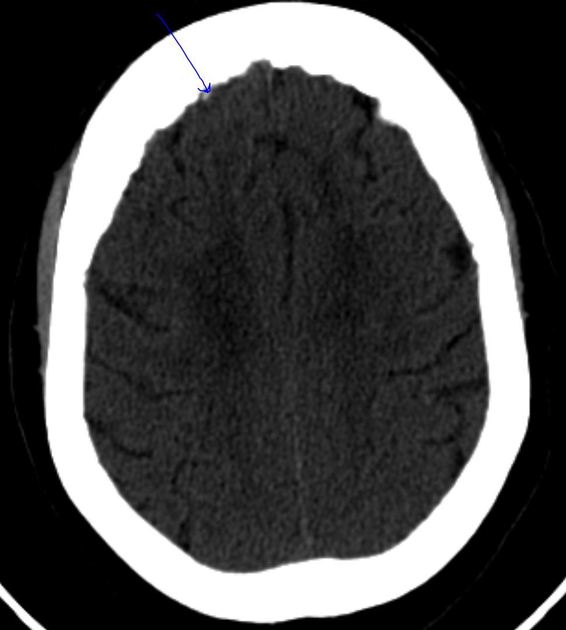
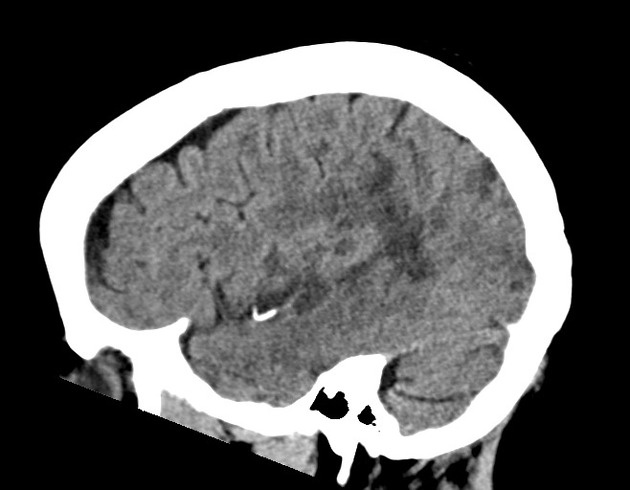
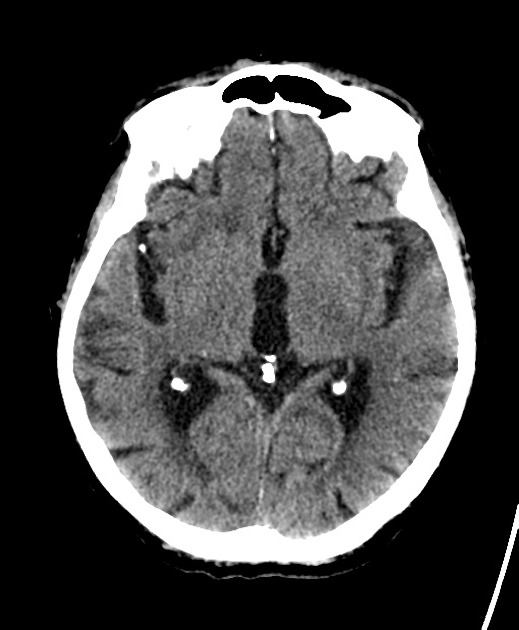
Calcified cerebral emboli are generally small in size, with a diameter of 2-3 mm 1.
Aetiology
Causes include 1-5:
-
spontaneous (~90%)
calcific aortic stenosis (most common)
calcified carotid, vertebral, brachiocephalic, and aortic arch plaques
-
iatrogenic
complication of procedures such as cardiac valve or coronary artery surgery
complications of carotid artery intervention (endarterectomy or endovascular stenting)
idiopathic
Radiographic features
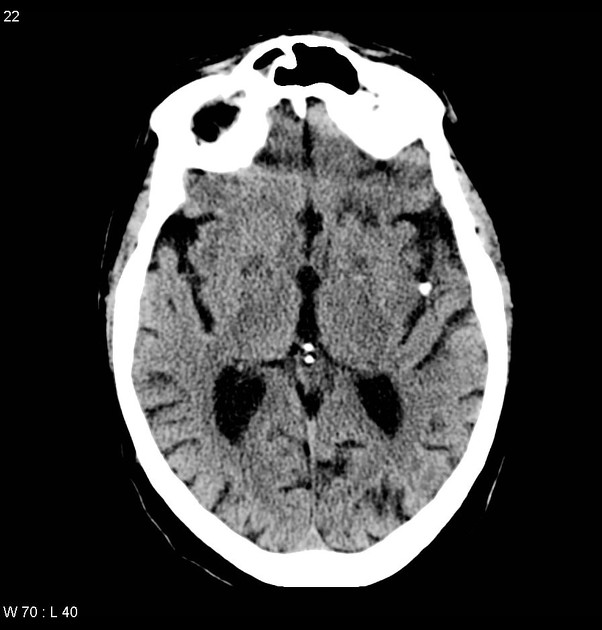
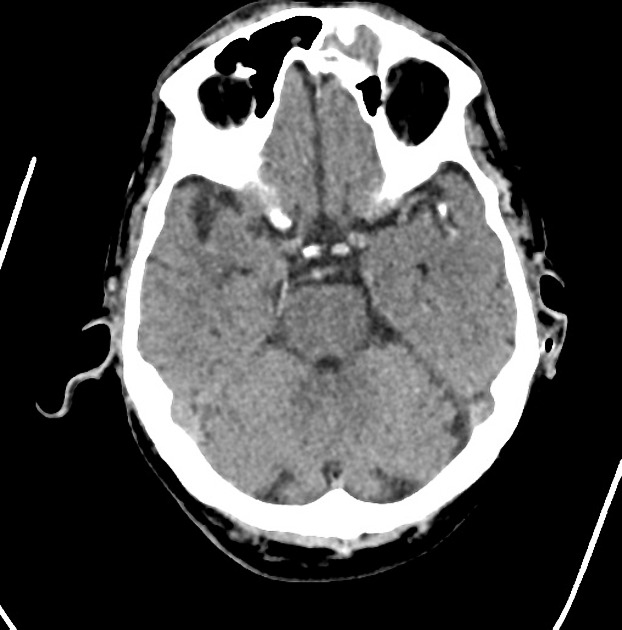
CT
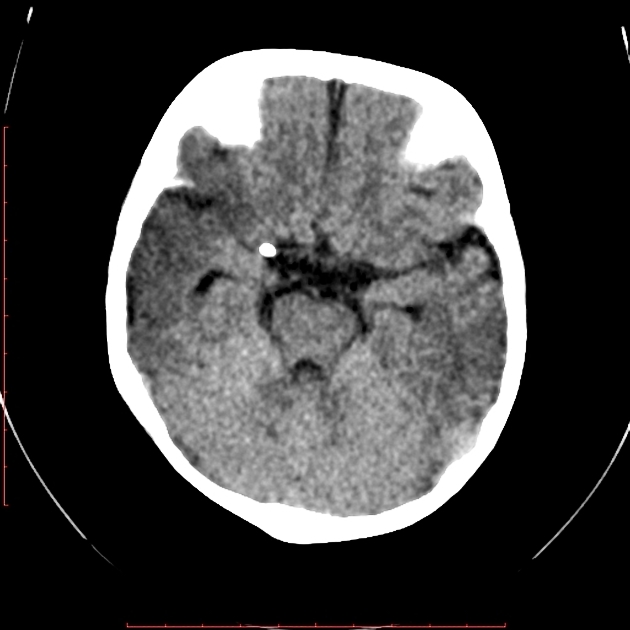
These emboli, having a calcified component, are hyperdense on non-contrast CT 1-3. If multiple are present, the salted pretzel sign may be seen 10.
Moreover, it may be of therapeutic and prognostic significance to differentiate this hyperdensity from that of a "regular" intramural thrombus (see hyperdense MCA sign and MCA dot sign) by observing the shape and by measuring the radiographic density of the embolus 1:
calcified cerebral emboli tend to have a round or ovoid shape, in comparison to "regular" thrombi which tend to fill up the vessel in a tubular configuration 1
with region-of-interest density measurements, calcified cerebral emboli are higher attenuation (~160 HU) in comparison to "regular" thrombi which are typically 50-70 HU 1
However, once calcium is suspected (especially if found incidentally), it is important to differentiate it from mimics such as haemorrhage, vessel wall calcification, infection (e.g. neurocysticercosis), cavernomas, or other causes of vascular intracranial calcification 1-3.
CT angiography
As these emboli are hyperdense on CT, they may appear isodense to the iodinated contrast used in CT angiography, which may give the impression that the vessel is patent when it really is not, especially in early-phase images 6. This has been described in one case report as "pseudo-patency" 6.
MRI
Although MRI is more sensitive than CT for detecting acute ischaemic stroke 7, CT is generally considered superior to MRI for detecting calcified cerebral emboli themselves both in terms of its accessibility and sensitivity 7. SWI filtered-phase imaging may be useful to confirm CT findings 15.
Treatment and prognosis
Stroke management guidelines do not make a distinction between calcified and "regular" non-calcified cerebral emboli with regard to thrombolysis 7, and there is mixed case series-level evidence regarding its effectiveness, although the consensus opinion is that it is less effective compared to patients with non-calcified cerebral emboli 2,7,8,16. Endovascular clot retrieval is also less effective with reduced angiographic reperfusion and less improved initial clinical outcomes, however, long-term functional outcomes and mortality may be comparable to patients with non-calcified cerebral emboli, and thus, this treatment should be strongly considered in appropriate candidates 13,14.
In terms of prognosis, calcified cerebral emboli may be a risk factor for recurrent stroke, with one study finding that nearly half of all patients had repeat embolic ischaemic stroke 1. Thus, it is paramount to also investigate for and treat any causative lesions (e.g. calcific aortic stenosis) in order to prevent recurrence 1.
History and etymology
Calcified cerebral emboli were first noted radiographically by Douglas H Yock, an American radiologist, in his 1981 seminal paper 9.
Differential diagnosis
-
vascular hyperdensity
hyperdense artery of thromboembolism
myelography contrast (e.g. Lipiodol) spread to cranial subarachnoid space 11
bone cement embolism 12
-
parenchymal hyperdensity
oligodendroglioma (especially in the setting of subacute infarction)
infections (e.g. neurocysticercosis, cerebral sparganosis, etc.)







 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.