Colitis cystica profunda or proctitis cystica profunda is a benign condition characterised by gastrointestinal submucosal mucinous cysts 1.
On this page:
Epidemiology
This is a rare condition related to solitary rectal ulcer syndrome and mucosal prolapse syndrome, which have an estimated incidence of 1:100,000 per annum 2. It is most common in 30-40 year old men 6,7.
Diagnosis
Cysts are readily apparent on MRI or transrectal ultrasound. At digital examination or endoscopy, bulging of the mucosa may be mistaken for malignancy.
Clinical presentation
Patients may present in the third or fourth decades with rectal bleeding, mucous discharge, tenesmus, constipation, or diarrhoea 6,7.
Lesions are firm on rectal digital examination and appear polypoid or sessile on endoscopy 1. The overlying mucosa may be normal, oedematous or ulcerated. Lesions are typically anterior and lie within 5-12 cm of the anal verge 6,7.
Pathology
Aetiology
The pathogenesis is unknown although is thought to related to a congenital or acquired (e.g. inflammatory, infectious, traumatic or ischaemic) mucosal muscle weakness, resulting in embedment of mucosal epithelium into the submucosa 6. Mucin is secreted into the cyst and occasionally infiltrates the submucosa.
Location
The rectum is the most common location (~70% 7) followed by the colon (~15% 7) although submucosal mucous cysts can occur in the stomach (gastritis cystica profunda), small intestine (enteritis cystica profunda), and colon 3,4,6.
Macroscopic appearance
Lesions can be ulcerative, polyploid, or sessile/flat 6,7.
Microscopic appearance
Variably sized and shaped submucosal mucous-filled cysts lined by flattened or columbar epithelial cells without malignant changes 6,7.
Associations
radiation enteritis 6
Radiographic features
Submucosal mucin cysts are readily apparent on TRUS or MRI and the bowel wall may otherwise appear normal.
Ultrasound
Mucin cysts in the submucosa generate low-level echoes on TRUS with distal acoustic enhancement 1.
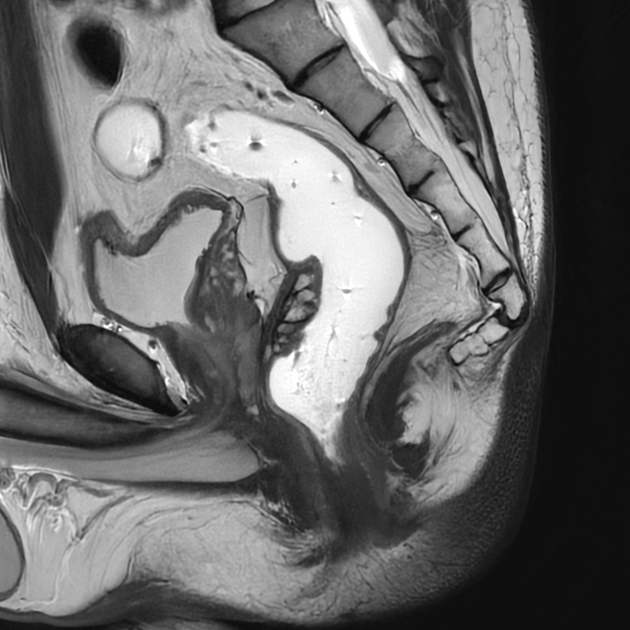
MRI
Associated dyssynergy or prolapse may be apparent on MR defaecography 5.
Signal characteristics
T1: submucosal low signal 2,6
T2: submucosal high signal 2,6
DWI/ADC: facilitated diffusion 6
T1C+: no significant enhancement 6
Treatment and prognosis
Treatment usually includes the following steps 1,6,7:
high-fibre diet to avoid straining
medications, e.g. glucocorticoids
local excision
surgical repair of rectal prolapse
History and etymology
This condition was first described by Stark in 1766 and given the name "colitis cystica polyposa" by Virchow in 1863 before finally being given its current name "colitis cystica profunda" by Goodall and Sinclair in 1957 6.
Differential diagnosis
Misdiagnosis as rectal cancer can lead to unnecessary abdominoperineal resection 1.





 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.