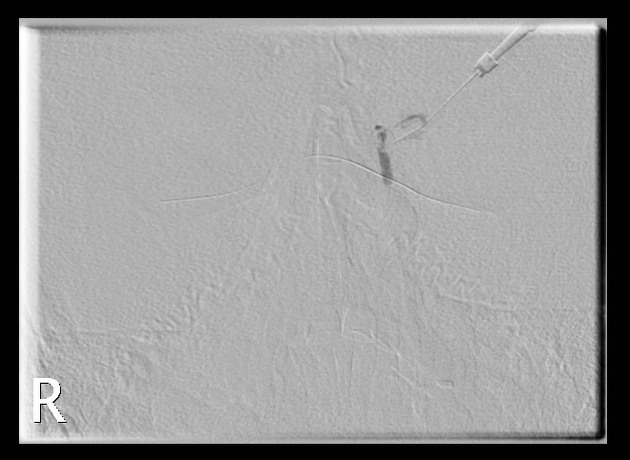
Dacryocystography (DCG) is a fluoroscopic contrast examination of the nasolacrimal apparatus. The nasolacrimal duct is cannulated enabling iodinated contrast to be instilled into the nasolacrimal system.
On this page:
Indications
The most frequent indication is epiphora: excessive tearing or watering of the eye(s) 3. DCG is mainly to locate the site of obstruction in the lacrimal drainage system, to differentiate canalicular from proximal sac obstruction, and detect the presence of stenotic segments that cannot be passed by a cannula 4.
The procedure is not recommended if an acute infection of the lacrimal system is suspected 5.
Types
There are several ways of performing a DCG 4:
conventional DCG
distension DCG
macrography DCG
seriography DCG
digitally subtracted DCG (DS-DCG)
kinetic conventional DCG
real-time DS-DCG
three-dimensional rotational DCG (3DR-DCG)
Technique
Equipment is similar to that used to perform a sialogram.
One suggested technique:
patient in the supine position 5
similar projection to an OM view in most cases
acquisition of a preliminary control film to confirm patient positioning and exposure
dilate the lacrimal punctum to insert the cannula. The cannula should be sited inside the canaliculus, near the punctal opening, so proximal obstruction can be seen if any 6.
non-ionic iodinated contrast injection into a cannulated duct, avoiding air bubbles
acquire images, whilst asking the patient to look straight ahead to avoid blinking
post-removal of cannula an erect view may be useful in diagnosing functional blocks
CT and MRI dacryocystography have also been described 1,2.
History and etymology
Dacryocystography was first performed by A E Ewing in 1909. He used bismuth subnitrate to demonstrate a lacrimal abscess cavity 3.





 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.