Developmental venous anomaly (DVA), also known as cerebral venous angioma, is a congenital malformation of veins that drain normal brain. They were thought to be rare before cross-sectional imaging but are now recognised as being the most common cerebral vascular malformation, accounting for ~55% of all such lesions.
A DVA is characterised by the caput medusae sign of veins draining into a single larger collecting vein, either a dural sinus or a deep ependymal vein. The appearance has also been likened to a palm tree.
On this page:
Epidemiology
DVAs are very common as an incidental finding, with an estimated prevalence of 3-9% on contrast-enhanced MRI scans 13.
Associations
lesions are usually solitary (75%) 2, except in blue rubber bleb naevus syndrome
~20% (range 8-33%) of cases 2 are associated with cavernous malformations and are referred to as mixed vascular malformations
venous malformations of the head and neck 2
cortical dysplasia (uncommon) 7
Clinical presentation
Developmental venous anomalies are usually incidental findings. However, patients can present with intracranial haemorrhage (1-5%). An association has also been described with ischaemic stroke and epilepsy 8.
Pathology
The aetiology of developmental venous anomalies remains uncertain but may relate to arrested development of venous structures 2,3.
Location
The most common locations are:
frontoparietal region (36-64%) 1, usually draining towards the frontal horn of the lateral ventricle
cerebellar hemisphere (14-27%) draining towards the fourth ventricle
However, DVAs can be seen anywhere, draining either superficially or deep.
Microscopic appearance
Histologically they consist of a number of abnormally thickened veins with normal feeding arteries and capillaries 3.
Radiographic features
Developmental venous anomalies are seen on both CT and MRI as a leash of vessels draining towards a central vein.
CT
If large, the draining vein may be seen on non-contrast CT and is confirmed with contrast administration as a linear or curvilinear enhancing structure.
Dystrophic calcifications may be seen associated in up to 10% of the cases 9. This can be particularly prominent in the basal ganglia and thalami resulting in unilateral calcification 10,11.
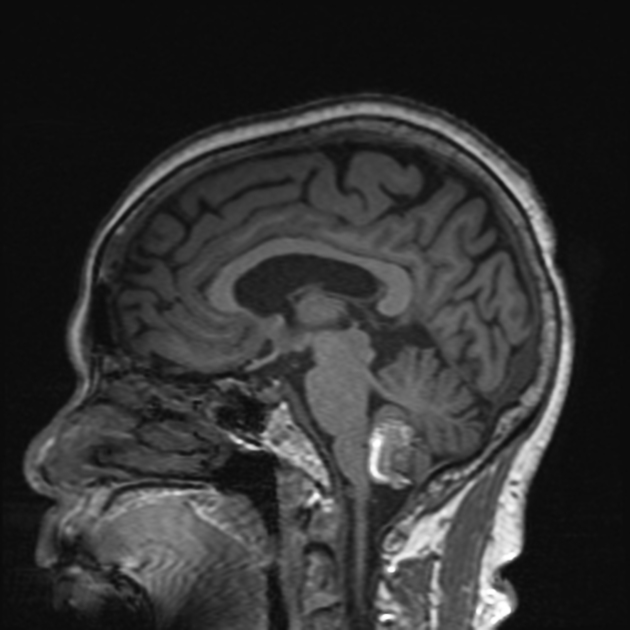
MRI
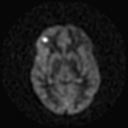
Developmental venous anomalies are often visible on most sequences but can be subtle and are most easily seen on postcontrast T1 sequences and susceptibility weighted imaging (SWI). If there is an associated cavernous haemangioma, then susceptibility weighted sequences will be most sensitive to this component.
Additionally, in ~10% of cases, high T2/FLAIR signal can be seen in the surrounding white matter; the aetiology is not clear but may be due to gliosis, oedema or leukoaraiosis 12.
SWI is the preferred sequence in venous anomalies and proved to have better detectability of venous structures than conventional T2*-weighted imaging. Signals on SWI are not compromised by low-velocity venous flow. Therefore, SWI has successfully demonstrated low-flow vascular formations such as DVA. The signal intensity of veins will be low on SWI images but will vary on phase imaging depending on the vendor. It will, however, be the same as other veins and the opposite of calcification.
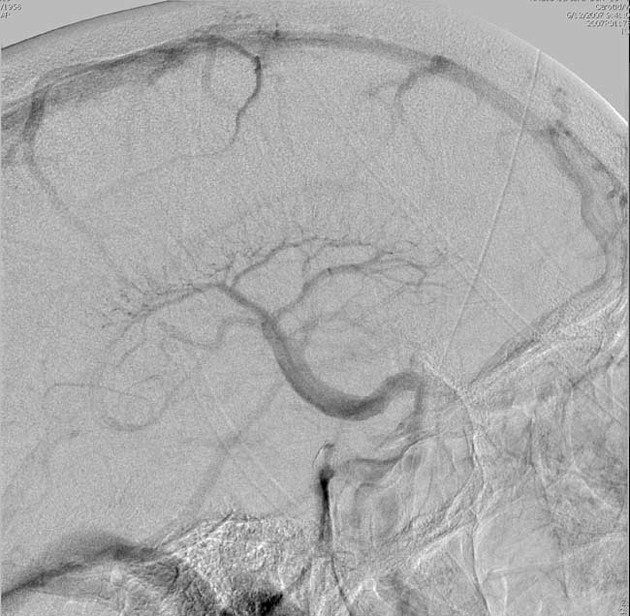
Angiography (DSA)
Angiographically, the caput medusae appearance (collection of dilated medullary veins converging in an enlarged transcortical or subependymal collector vein) is pathognomonic and seen only in the venous phase. Arterial phase appears normal although late capillary blush may be present. No shunting is present.
Treatment and prognosis
If isolated developmental venous anomalies require no treatment. If part of a mixed vascular malformation then treatment will be predicated on the other component. Informing the surgeon of the presence of a DVA is, however, essential as cautery of the collecting vein can lead to venous infarction of the brain parenchyma it drains.
When isolated, developmental venous anomalies have a very low complication rate (0.15% per annum) mainly from spontaneous thrombosis of the collecting vein leading to venous infarction and haemorrhage.
A study has demonstrated that in exceedingly rare cases, the DVA can become symptomatic by various vascular complications. The authors suggested identification of the underlying pathomechanism by MR and DSA for proper management. The importance of the preserved integrity of the DVA itself still holds true 6.
Differential diagnosis
Generally, the appearances will be typical and no differential should be offered. In some instances, imaging appearances may be atypical or be confounded by concurrent pathology (e.g. haemorrhage). In such cases it is worth considering:
dural sinus thrombosis or dural arteriovenous fistula with collateral transparenchymal drainage
Sturge-Weber syndrome with leptomeningeal angiomatosis
demyelination may also have enlarged medullary veins
Practical points
think of an associated cavernoma when a developmental venous anomaly is found in the context of an intraparenchymal haemorrhage investigation, as isolated DVAs rarely bleed
developmental venous anomalies can be subtle on many MRI sequences; T1 C+ and SWI are most sensitive























 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.