Divry van Bogaert syndrome is a familial juvenile-onset syndrome characterised by livedo racemosa, juvenile ischaemic stroke, juvenile cerebral white matter disease leading to premature dementia, and epilepsy.
On this page:
Clinical presentation
juvenile ischaemic stroke
early-onset cognitive impairment
livedo racemosa: a net-like violaceous discoloration of the skin, persistent even after warming of the limbs
Diagnostic criteria
hereditary
juvenile dementia or juvenile-onset of progressive cognitive impairment
juvenile ischaemic stroke (defined as a stroke <45 years)
juvenile onset of leukoaraiosis
livedo racemosa
cerebral angiogram showing peripheral arterial occlusions and peripheral angiomatosis
exclusion of other reasons for stroke in young adults (e.g. CNS vasculitis, repeated thromboembolism, thrombophilia, CADASIL, etc.)
Radiographic features
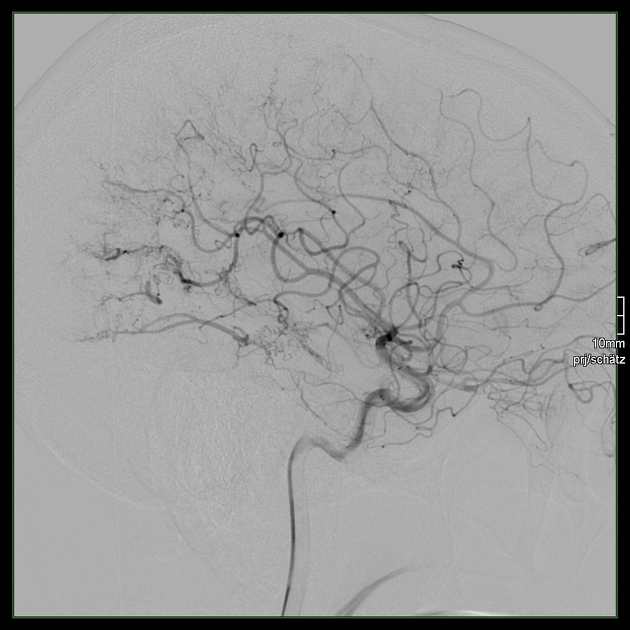
Angiography (DSA)
Typical features include:
extensive, multifocal occlusions of the peripheral, small- and medium-sized cerebral arteries
-
extensive neovascularisation, with a network of thin and irregular collateral vessels giving an 'angiomatous appearance' of the peripheral circulation
leptomeningeal anastomoses are present: small arterial connections connecting the terminal cortical branches of the major arteries MCA, ACA and PCA
transdural anastomoses are present: connecting the ECA and ICA territory
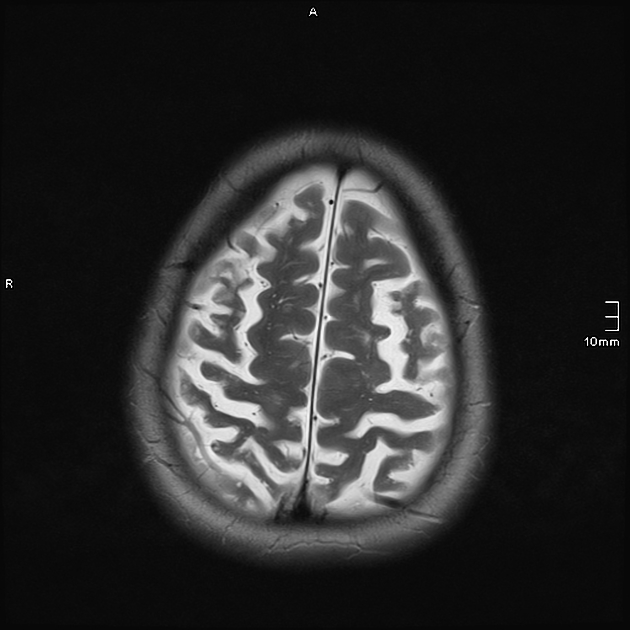
MRI
MRI brain reveals diffuse leukoaraiosis and/or acute ischaemic strokes.
Treatment and prognosis
There is no effective treatment, but antiplatelet therapy is usually advised, similar to management in many other cerebral arteriopathies.
History and etymology
The syndrome was first described by Paul Divry (1889-1967) and Ludo van Bogaert (1897-1989), Belgian physicians, in 1946 2.
Differential diagnosis
-
less severe cerebrovascular involvement
cerebral angiomatosis, juvenile cognitive impairment, and epilepsy are rare
there usually is no positive familiar history for the disease, although familial cases have been described
approximately half of Sneddon syndrome patients also have antiphospholipid syndrome
skin biopsy can be diagnostic
-
DSA typically shows occlusion of proximal, large-sized cerebral arteries
there are multiple very small perforator collaterals proximally around the occlusions at the circle of Willis giving a 'cloudy', 'puff of smoke' appearance, unlike Dirvy van Bogaert syndrome which has distal/peripheral angiomatous processes




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.