Facet joint arthropathy/arthrosis is a common cause of low back pain and is most commonly due to osteoarthritis. It occurs from facet joint chondral loss, osteophyte formation and hypertrophy of the articular processes that may cause spinal canal stenosis in severe cases.
Facet joint arthropathy can occur anywhere in the spine and has potentially multiple causes, however, this article focuses on degenerative lumbar facet joint arthropathy.
On this page:
Epidemiology
Facet joint arthropathy is a common finding, especially in the lumbar spine, that increases in extent and severity with increasing age. It accounts for ~30% (range 15-45%) of low back pain 8. Approximately 50% of adults <30 years and ~95% of adults >60 years have some degree of facet arthropathy 8. Men have a higher prevalence compared to women ref.
Diagnosis
History and diagnosis can suggest facet joint arthropathy as a cause for back pain. Facet joint injections (intra-articular or median branch blocks) may confirm facet joint-related back pain 10 but there are high false-positive rates 7,8. Some consider facet joint arthropathy as a cause for low back pain as a diagnosis of exclusion after discogenic causes and nerve root compression has been excluded 7.
Clinical presentation
Patients can present with "facet joint syndrome" of low back pain radiating to the buttock, groin or thigh (often referred to as "pseudoradicular") but not below the knee. Symptoms can be unilateral or bilateral and there are no neurological deficits 7,8,. Clinical examination techniques include the Kemp test.
Pathology
Aetiology
Osteoarthritis is the most common cause of facet joint arthropathy but other causes include rheumatoid arthritis, ankylosing spondylitis and septic arthritis 6,8.
The facet joints comprise the posterior elements of the "three-joint complex" (with the intervertebral disc forming the anterior element) that describes a spinal segment. Facet joint degeneration occurs as part of this complex, and as the disc degenerates more load will shift posteriorly and facet joint osteoarthritis will subsequently develop 6.
Degenerative facet joint arthropathy can rarely occur without disc degeneration and specific causes (e.g. specific rotational activities such as golf) should be considered 6.
Classification
Two classification systems are in routine clinical use (c.2018) 8:
Pathria grading scale: plain radiograph and CT
Weishaupt grading system: CT and MRI
Radiographic features
Radiography is not particularly sensitive for detecting mild or moderate facet joint osteoarthritis and is best viewed as a screening tool 6. MRI and CT can both show morphological changes although MRI may underestimate severity 8. SPECT-CT is best at identifying patients with facetogenic low back pain who may benefit from facet joint injections 7.
Findings typical of osteoarthritis are seen in all modalities 8:
joint space narrowing
subchondral sclerosis/bone erosions
Plain radiograph
Oblique views are preferred over standard AP and lateral views. Additional features include joint capsule calcification and vacuum phenomenon 8.
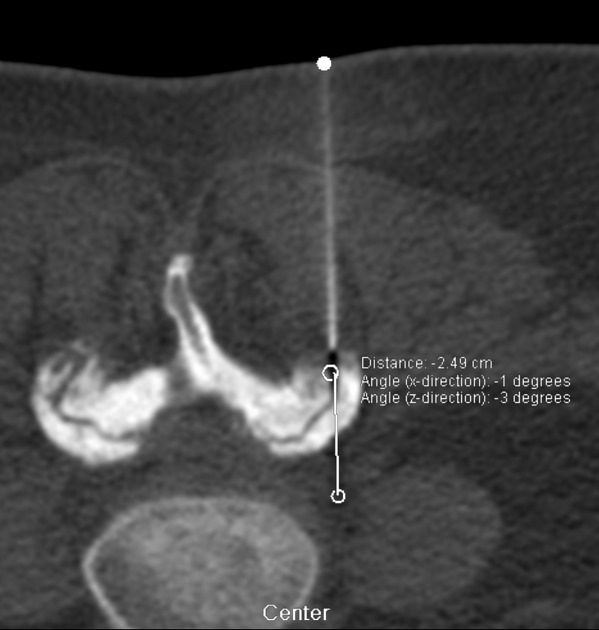
CT
Features are similar to plain radiographs although with increased sensitivity 8.
MRI
Additional features seen on MRI are juxta-facet cysts, subchondral bone oedema and facet joint effusion. Synovitis can be diagnosed on post-contrast imaging 8,10.
Nuclear medicine
Bone scintigraphy
On planar and SPECT imaging, increased uptake can be shown at the facet joint reflecting increased osteoblastic activity related to synovitis and bone remodelling 7,10.
PET
18-F FDG PET-CT demonstrates uptake in symptomatic facet joints even when no morphological degenerative changes are seen 9.
Treatment and prognosis
Pharmacologic therapy and physiotherapy are first-line treatments. Interventional treatments include facet joint injection, medial branch block, and neurolysis (e.g. radiofrequency ablation, cryoneurolysis, chemical neurolysis) are among the treatment options 7,8. Patients with positive SPECT findings have a better response to facet joint injections 10.
Differential diagnosis
The differential diagnosis of facet joint syndrome depends on referred pain distributions but includes 8:
hip pathology, e.g. hip osteoarthritis, trochanteric bursitis
sacroiliac joint arthropathy





 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.