Fibrosing mediastinitis is a rare non-malignant acellular collagen and fibrous tissue proliferative condition occurring within the mediastinum. On imaging, the condition can sometimes mimic malignancy.
On this page:
Epidemiology
Although it can potentially present at any age, it typically presents in young adults.
Associations
Behçet disease (rare) 10,11
-
other autoimmune conditions:
Clinical presentation
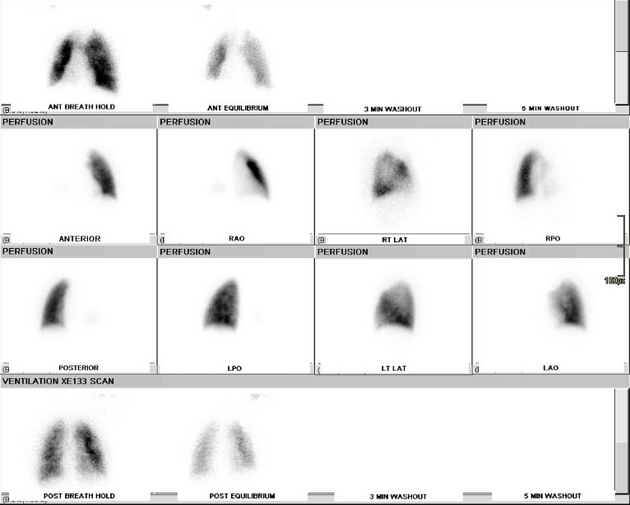
Affected patients usually present with signs and symptoms of obstruction or compression of the superior vena cava, pulmonary veins or arteries, central airways, or oesophagus and may complain of broncholithiasis.
Pathology
It is characterised by chronic inflammation and excessive fibrosis of mediastinal soft tissues. This may lead to compression and sometimes occlusion of mediastinal structures. There are two main pathological types:
focal: ~80% 5,6
diffuse: ~20%
Aetiology
idiopathic: most cases 12, thought to be a form of IgG4-related disease 17
-
infection:
Histoplasma capsulatum infection (histoplasmosis): common in the United States and often gives a localised pattern 8
Mycobacterium tuberculosis infection (pulmonary tuberculosis) 5
concurrent intrathoracic malignancy 5
sarcoidosis 14
radiation therapy
drugs: e.g. methysergide therapy 8
Radiographic features
Plain radiograph
Can be subtle and may be seen as a non-specific widening of the mediastinum. There can be distortion and obliteration of normally recognisable mediastinal interfaces or lines. There may also be mediastinal and/or hilar calcification (~85%) which is more common in the localised type 3.
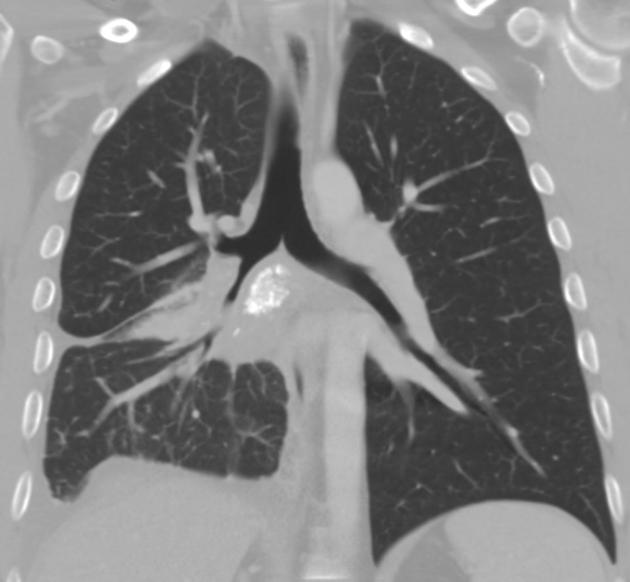
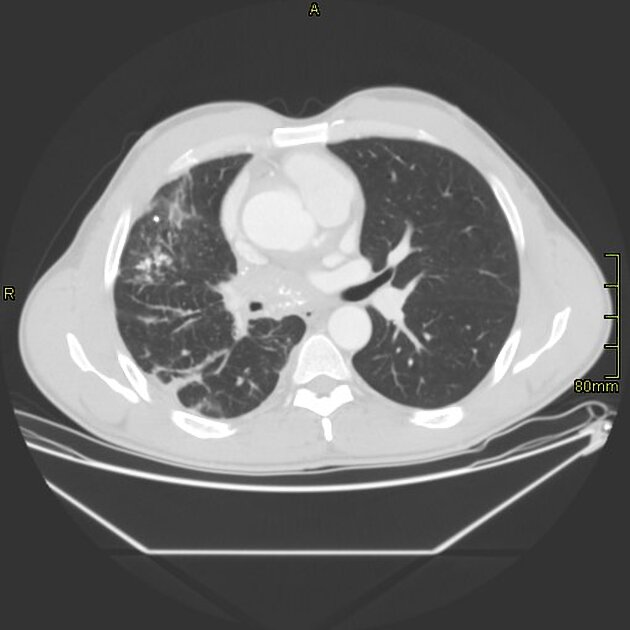
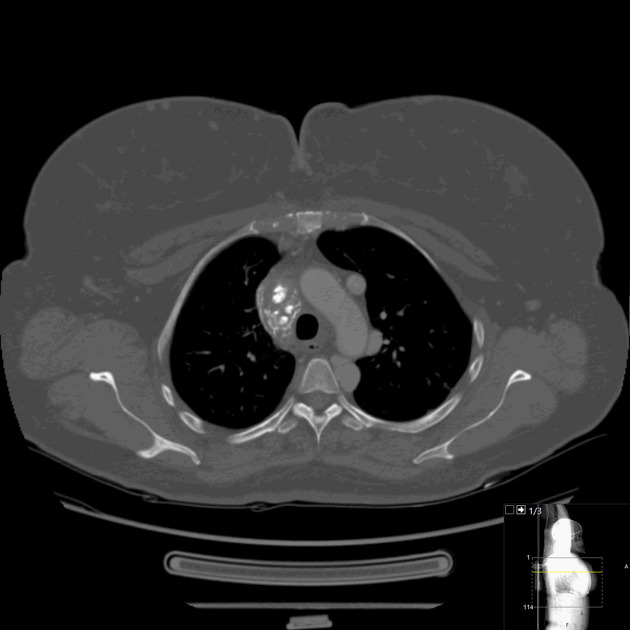
CT
The exact appearance can be variable and dependent on the pattern of involvement. Typically affects the middle mediastinum and may show:
mediastinal or hilar mass: especially in localised disease
soft-tissue attenuation which obliterates normal mediastinal fat planes and encases or invades adjacent structures: diffuse form
Other findings include:
calcifications of the central mass or associated lymph nodes: especially if there has been preceding histoplasmosis
areas of pulmonary opacity 2
endobronchial calcification with atelectasis of the associated segment or lobe
associated pulmonary granuloma reflecting the original cause like healed granuloma from tuberculosis or histoplasmosis
engorged bronchial arteries due to vascular compromise
local lung changes: prominent interstitial pattern (segmental and/or diffuse) and crazy paving secondary to compressed veno-lymphatic pathways.
MRI
The pattern of involvement is essentially similar to CT. Signal characteristics include:
T1: typically heterogeneous but overall isointense to muscle
T2: variable with both high 3 and low 2,3 signal within the same lesion
T1 C+ (Gd): may show heterogeneous enhancement
Treatment and prognosis
Fibrosing mediastinitis can have an unpredictable course, with both spontaneous remission or exacerbation of symptoms being reported.
It usually tends to be slowly progressive. There are three possible avenues for treatment: systemic antifungal or corticosteroid treatment, surgical resection, and local therapy for complications.
Surgical resection of the affected region could be considered with localised disease. Some patients with the diffuse pattern show radiographic evidence of improvement with steroid therapy.
Complications
superior vena cava (SVC) compression/obstruction/thrombosis
airway stenosis/obstruction 15
mediastinal perivascular pseudoaneurysms 18





 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.