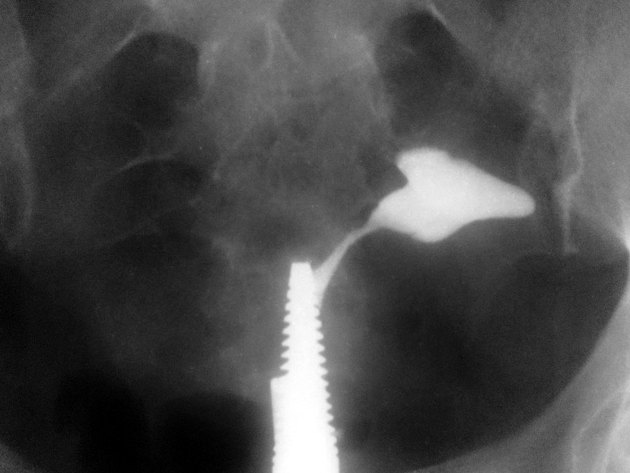
A hysterosalpingogram (HSG) is a fluoroscopic examination of the uterus and the fallopian tubes, most commonly used in the investigation of infertility or recurrent spontaneous abortions.
On this page:
Indications
infertility: to assess uterine morphology and tubal patency
Contraindications
pregnancy
active pelvic infection
recent uterine or tubal surgery
Procedure
Technique
-
the procedure should be performed during the proliferative phase of the patient’s menstrual cycle (days 6-12) when the endometrium is thinnest
this improves visualisation of the uterine cavity and also minimises the possibility that the patient may be pregnant 1
if there is any uncertainty about the patient’s pregnancy status, a beta hCG is warranted before commencing
after an antiseptic cleaning of the external genital area, a vaginal speculum is inserted with the patient in the lithotomy position; the cervix is cleaned with an aseptic solution
-
catheterisation of the cervix is then performed; the type of device used depends on local practice preferences, and the main options are:
-
a 6 Fr Foley catheter with balloon inflation
-
a Foley catheter has several technical disadvantages, such as difficult insertion in an:
angulated or problematic cervix
acutely anteverted or retroverted uterus
cervical stenosis
highly positioned cervix due to pelvic adhesions, previous surgery, or uterine leiomyoma
a Foley catheter should be placed just beyond the internal os of the cervix; if the catheter is placed within the cervical canal, it can be easily dislodged
inadequate seal of the balloon with the internal os will result in leakage of the contrast through the cervical canal, generating inadequate intrauterine pressure to push the contrast out of the bilateral fallopian tubes; this results in a false positive result of fallopian tube blockage 2
-
-
a hysterosalpingography catheter or metal acorn-tipped cannula 3 (e.g. Leech Wilkinson, Margolin, etc.)
a Leech Wilkinson catheter allows the passage of the angiographic tip to perform Fallopian tube clearance 10
a tenaculum is also used to provide traction on the cervix
a Margolin catheter has a silicon tip that can be inserted within a narrow cervical lumen
a cervical vacuum cup
-
whatever the device, it should be primed with contrast before insertion to avoid the introduction of gas bubbles which may provide a false positive appearance of a filling defect
-
water-soluble iodinated contrast is subsequently injected slowly under fluoroscopic guidance
some radiologists use iodinated oil (Lipiodol) as contrast when the indication is for lack of fertility, as some authors report increased fertility after its use; however, this remains controversial 8
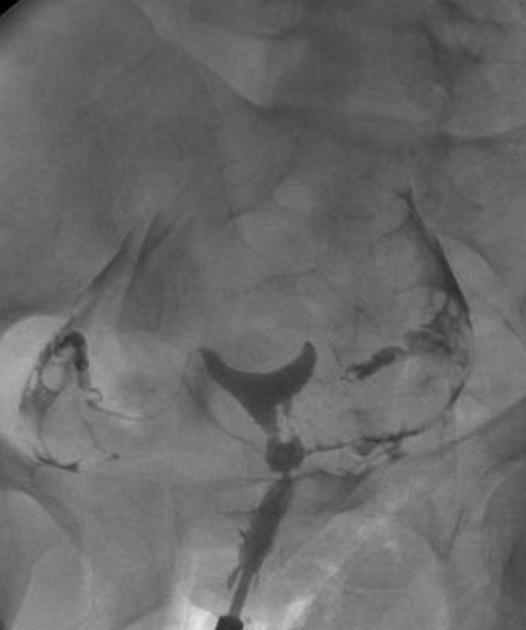
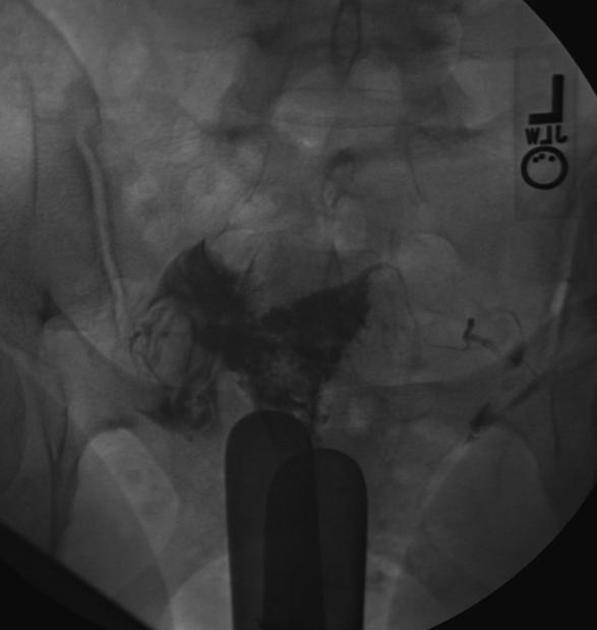
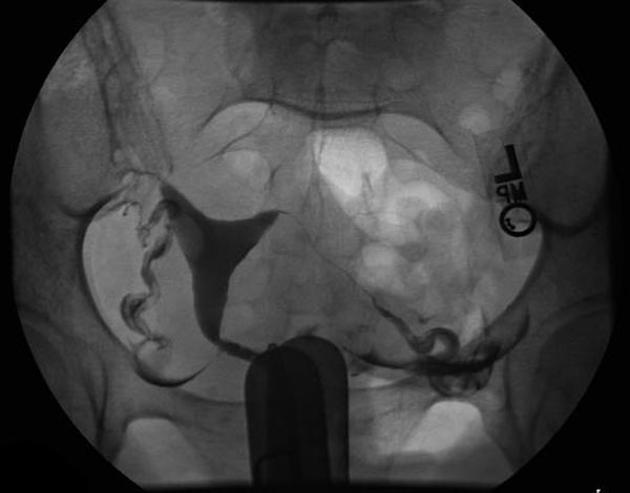
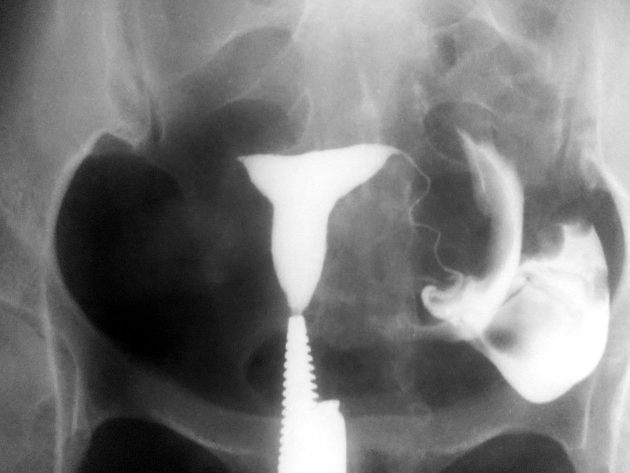
a typical fluoroscopic examination includes a preliminary frontal view of the pelvis, as well as subsequent spot images that demonstrate the uterine endometrial contour, filled fallopian tubes, and bilateral intraperitoneal spill of contrast to establish tubal patency
Complications
Common but self-limiting
abdominal cramping
per vaginal spotting
Rare but serious
pelvic infection
contrast reaction
tubal or uterine perforation
Detectable pathology
Conditions that may be detected with hysterosalpingography include:
Uterine
submucosal uterine fibroids
Tubal
-
obliteration of fallopian tubes: usually secondary to previous pelvic inflammation
it must be differentiated from incomplete tubal opacification due to tubal spasm, or underfilling of the uterus with contrast 9
tubal spasm 6: can be physiological
salpingectomy















 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.