Impingement syndrome is a painful encroachment of joint motion caused by protruding bony or soft tissue structures.
On this page:
Epidemiology
Impingement syndromes are common and can occur at any age.
Risk factors
developmental osseous anomalies
overuse activity
trauma
Associations
tendinosis and tears
myotendinous injury
chondral and labral injury
Clinical presentation
The usual presentation of impingement syndrome is a painful reduction in the range of motion of the affected joint 1.
Pathology
The pathological correlate of impingement is a mechanical entrapment or encroachment of soft tissue structures between bony formations of a joint.
Aetiology
Bony structural abnormalities due to:
developmental anomalies
repetitive microtrauma/overuse
Location
Typical locations are the following joints 1:
Classification
Internal impingement: refers to an intraarticular impingement, the affected structures are within the joint e.g. femoroacetabular impingement, anterior, anteromedial, anterolateral, posterior or posteromedial ankle impingement, subcoracoid impingement
External impingement: refers to an extra-articular impingement, of which the affected structures lie outside the joint e.g. ischiofemoral impingement, extra-articular lateral hindfoot impingement
Radiographic features
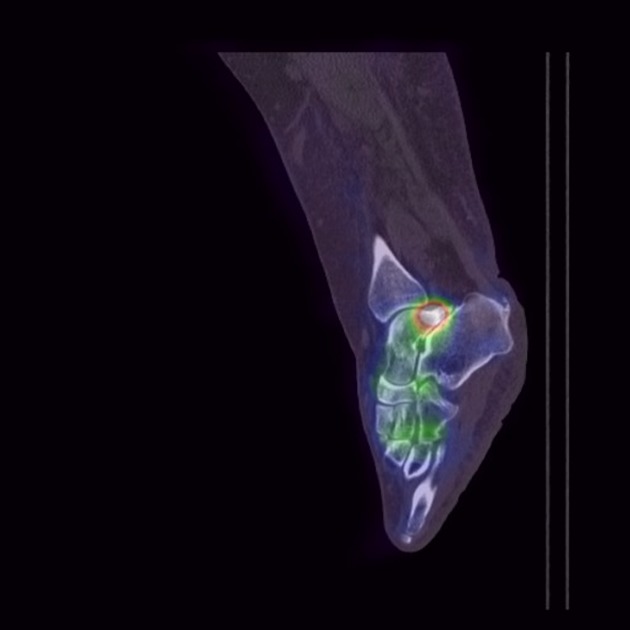
Plain radiograph/CT
Depiction of predisposing osseous abnormalities e.g.:
os acromiale, acromion type III, decreased coracohumeral distance
cam and/or pincer morphology, decreased ischiofemoral distance
anterior/anteromedial tibiotalar osteophytes, flat foot, hindfoot valgus
Ultrasound
A dynamic ultrasound examination allows the demonstration of the abutment or narrowing effect on the impinged soft tissue structures 1.
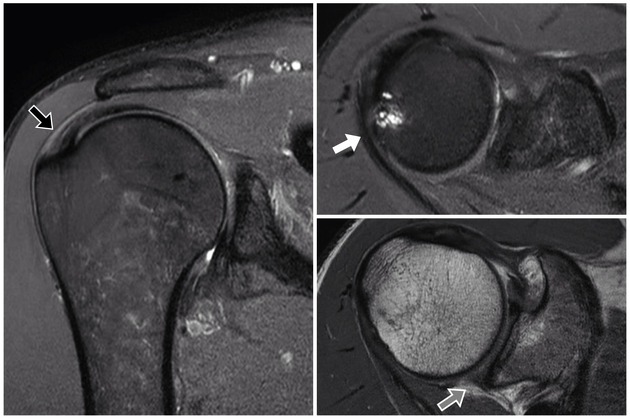
MRI
In addition to osseous morphologies or abnormalities, MRI can depict a stress response of the affected bony and soft tissue structures as e.g. bone marrow-like signal of the affected bone or signs of tendinosis, muscle oedema or tears of the encroached tendinous and/or myotendinous structures 1. Furthermore, it can show sequelae as ligamentous injuries, bursitis, capsulitis, chondral or labral injury and muscular changes such as atrophy or fatty degeneration.
Treatment and prognosis
Treatment depends on the location and extent of symptoms. It typically includes exercise therapy, activity modification, taping, physical and manual therapy, temporary immobilisation as well as nonsteroidal anti-inflammatory drugs, and guided injections of local anaesthetic or corticosteroids. Surgery is usually performed if conservative management fails or if complications have already occurred.






 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.