Infectious or septic tenosynovitis refers to an infection of the closed synovial tendon sheath 1-3.
On this page:
Terminology
The term infectious or septic tenosynovitis applies to tendons with a tendon sheath; for tendons without a tendon sheath with a paratenon, the term infective paratenonitis can be used to name the specific tendon 1.
Epidemiology
Risk factors
Risk factors of infectious tenosynovitis include 4,5:
Associations
Infectious tenosynovitis may be associated with the following conditions 1-5:
skin breach, puncture wound, laceration, ulceration
septic bursitis
Diagnosis
The diagnosis of infectious tenosynovitis can be made by a combination of typical clinical features of infection in the setting of characteristic imaging findings and can be verified by the culture of the purulent synovial fluid 1.
A synovial biopsy can be obtained in the setting of suspected granulomatous infection.
Clinical presentation
Symptoms of infectious tenosynovitis include swelling, erythema, tenderness, warmth and painful range of motion of the respective tendon 2. Laboratory studies may show increased inflammatory markers such as leukocyte count or C-reactive protein (CRP).
Complications
Complications of a soft tissue abscess include the following 2,3:
tendon necrosis or tendon disruption
Pathology
The underlying pathologic correlate of infectious tenosynovitis is an infection and/or pus within the tendon sheath sometimes also leading to adhesions and septations 1,2.
Etiology
Infectious tenosynovitis is usually a result of a contiguous spread from an underlying ulcer or septic arthritis or direct infection via skin breach 1,2. Less often it can happen due to hematogenous seeding 2.
Potential organisms of infectious tenosynovitis include pyogenic bacteriae, mycobacteria and fungi 2.
Location
The hand and wrist are the most common location of infectious tenosynovitis, especially the flexor compartment in the setting of pyogenic flexor tenosynovitis 2-4. Tendon infections have been also described for other sites including the wrist extensor tendons the flexor and extensor tendons of the foot and ankle 5,6 and the long head biceps tendon 7.
Radiographic features
On imaging, tenosynovitis is characterized by fluid within the tendon sheath, that may show different signal characteristics depending on whether pus, gas or blood products are present, which favor an infective cause over a pure inflammatory origin 1,2.
Plain radiograph
Plain x-rays are of limited value in the diagnosis of infective tenosynovitis but can display soft tissue swelling and/or gas or foreign bodies as a potential cause 2,3.
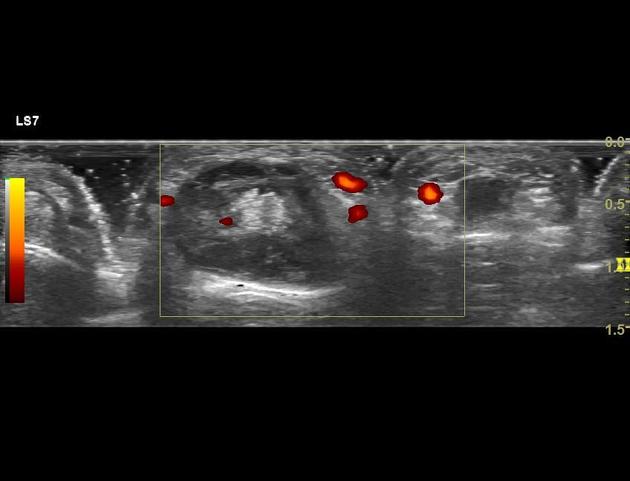
Ultrasound
Ultrasound may show synovial hyperemia and fluid distension of the tendon sheath 2,3.
CT
CT may demonstrate fluid and/or gas within the tendon sheath, synovial thickening and enhancement 2,3.
MRI
MRI is considered the preferred modality for the assessment of tenosynovitis and may show the following 1-3:
a complex, inhomogeneous fluid signal within the tendon sheath
soft tissue-edema like signal around the tendon sheath
synovial thickening with contrast enhancement
synovial adhesions/septations
thickened tendons with variable signal alterations and/or enhancement
Radiological report
The radiological report should contain a description of the following 1-3:
presence of tenosynovitis
presence of adhesions, gas, blood products within the tendon sheath
-
associated findings
ulcer, skin breach
overlying cellulitis/soft tissue swelling
adjacent bone erosion
joint effusion/septic arthritis
bursitis
foreign body
Treatment and prognosis
The management of infectious tenosynovitis is surgical and considered an emergency 2,4. Additional measures include administration of antibiotics, splinting and limb elevation.
Differential diagnosis
Conditions mimicking the radiological appearance of infectious tenosynovitis include 1,2:
inflammatory tenosynovitis




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.