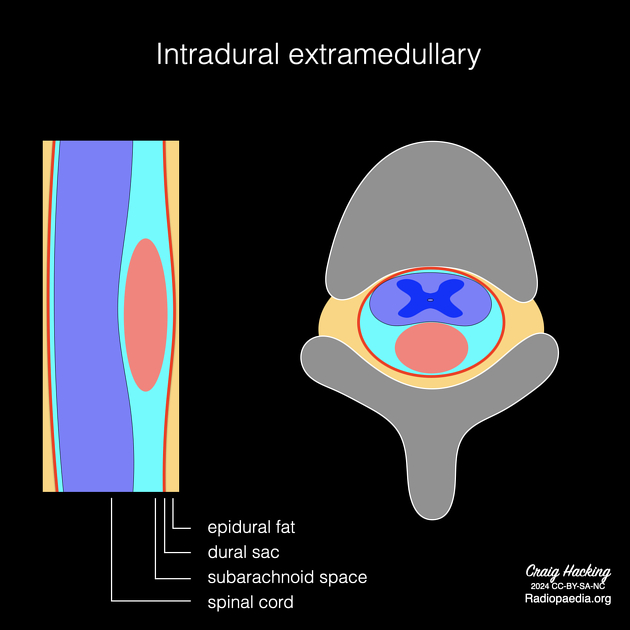
Intradural extramedullary neoplasms are located outside the spinal cord but within the dural sheath.
On this page:
Epidemiology
The majority (70-80%) of spinal canal tumours are intradural extramedullary 1.
Clinical presentation
Patients present with signs and symptoms of spinal cord or nerve root compression. Common presentations include weakness, localised back pain, radicular pain, sensory deficits, and gait ataxia.
Pathology
Aetiology
The most common primary intradural extramedullary neoplasms are meningioma (20-30%) and schwannoma (15-50%), followed by neurofibroma 1. Less common entities include solitary fibrous tumour/haemangiopericytoma and malignant peripheral nerve sheath tumour.
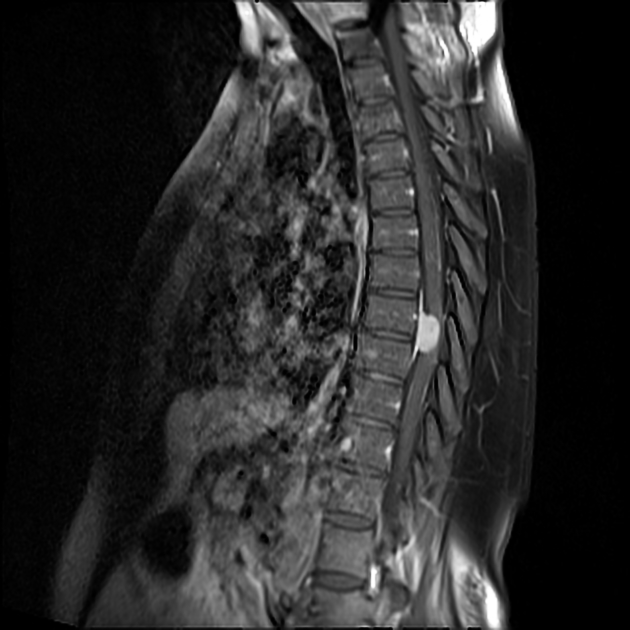
Leptomeningeal metastases are frequently seen (5-15%) in the setting of solid tumours (most commonly melanoma, small cell lung cancer, and breast cancer) and haematologic malignancies. In children, the most common intradural extramedullary neoplasms are drop metastases from primary brain tumours (most commonly medulloblastoma). In adults, the most common drop metastases are from glioblastoma.
The category includes primary neoplasms of the cauda equina region, but these have a distinct differential diagnosis, particularly the addition of myxopapillary ependymoma and, less commonly, neuroendocrine tumours (paraganglioma) arising from the filum terminale.
A useful mnemonic can be found here.
Radiographic features
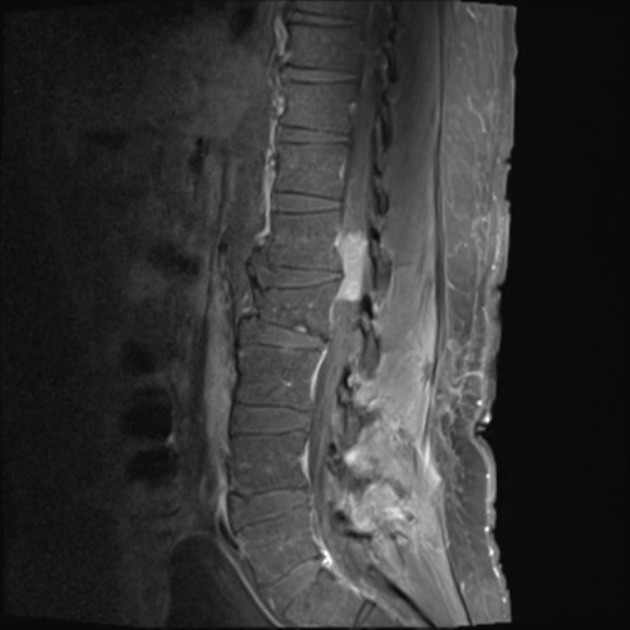
In general, a mass lesion is demonstrated within the spinal canal, sometimes with extension into the neural foramina and extradural paraspinal region (which is more suggestive of a nerve sheath tumour). When there is adequate contrast resolution of the cerebrospinal fluid (CSF) space, the mass can be localised within the dura but outside the spinal cord.
Plain radiograph
- may be normal
- may show bone erosion, remodelling, or sclerosis
- may show a paravertebral mass
CT
- may show bone erosion, remodelling, or sclerosis
- may show a paravertebral mass
- may show tumoural calcifications (especially meningioma)
Myelography
- deviation of the spinal cord away from mass
- ipsilateral cerebrospinal fluid (CSF) space enlargement surrounding the mass and contralateral CSF space effacement
- intradural filling defect outlined by sharp meniscus of contrast (“meniscus sign”)
- the subarachnoid space is blocked and CSF above the block remains unopacified
MRI
Contrast-enhanced MRI is the modality of choice to fully characterise these masses. The key benefits of MRI are greater sensitivity of detection and the ability to narrow the diagnostic differential by defining signal characteristics and the relationship of the mass to the cord, dura, and nerve roots. In addition, MRI can help in identifying secondary lesions and large feeding/draining vessels.
The appearance will vary depending on the histology and is thus discussed in depth in individual articles (see above list). Distinguishing features include the following 1,4,5:
- meningioma: dural involvement with dural tail sign, homogeneous contrast enhancement, ginkgo leaf sign
-
nerve sheath tumour: nerve root involvement, extradural neural foraminal extension with dumbbell appearance
- schwannoma: marked T2 hyperintensity, heterogeneous (cystic) when larger, displace nerve roots, round
- neurofibroma: marked T2 hyperintensity, encase nerve roots, fusiform or plexiform
- melanotic schwannoma: T1 hyperintensity, T2 hypointensity
- leptomeningeal metastasis: spinal cord margin or nerve root involvement (especially cauda equina) with multifocal nodular enhancement
- myxopapillary ependymoma: cauda equina region with sausage-shaped morphology
- neuroendocrine tumours (paraganglioma): cauda equina region with prominent flow voids, cap sign
Differential diagnosis
The differential for intradural extramedullary neoplasms includes non-neoplastic developmental mass lesions in this location:
-
intradural spinal lipoma
- fat signal intensity on MRI
-
spinal dermoid cyst
- calcification on CT
- heterogeneous T1 hyperintensity on MRI
-
spinal epidermoid cyst
- CSF signal intensity with restricted diffusion on MRI
-
spinal arachnoid cyst
- CSF signal intensity without restricted diffusion on MRI
- spinal neurenteric cysts
Uncommon appearances of degenerative disease can mimic a mass:





 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.