A jet or flame-shaped haemorrhage is a term sometimes used to describe an intraparenchymal haematoma adjacent to a ruptured arterial vascular malformation, such as aneurysms (most common) or dural arteriovenous fistulae or arteriovenous malformations 1,2. It usually is seen in combination with subarachnoid haemorrhages, intraventricular haemorrhages or subdural haemorrhages, although rarely they can be seen in isolation 3. It is particularly in this latter scenario that recognition of the shape is helpful in guiding additional imaging.
On this page:
Terminology
The use of the term "jet" or "flame" to describe haematomas is not very common in the published literature, and flame haemorrhage most commonly refers to a subset of retinal haemorrhages. Nonetheless, given the importance of this finding, it is worth using it as an aid memoir.
It should also be noted that the term flame-shaped haemorrhage has been used by some authors to denote the pattern of haemorrhage in venous infarcts 4.
Clinical presentation
The clinical presentation is highly variable, depending on the location and size of the haemorrhage.
Pathology
These haematomas result from the rupture of an aneurysm that abuts the surface of the brain and the pressure of the blood leaving the aneurysm dissects into the brain parenchyma. The pathophysiology of how some of these haemorrhages are isolated, without concurrent subarachnoid haemorrhage is not well understood, but it is hypothesised that adhesion between the aneurysm dome and the brain surface, due to inflammation or prior leakage creates a region where blood can rupture into the parenchyma without involving the subarachnoid space 3.
The same principle has been implicated in isolated subdural haematomas resulting from aneurysmal rupture 5.
Location
The location of the haemorrhage can be useful in predicting the location of the ruptured aneurysm.
-
inferomedial (gyrus rectus): ruptured ACOM/A1aneurysm
inferolateral (frontal operculum): ruptured M1 aneurysm
-
pole or temporal operculum: ruptured M1 aneurysm
medial: rupture PCOM aneurysm
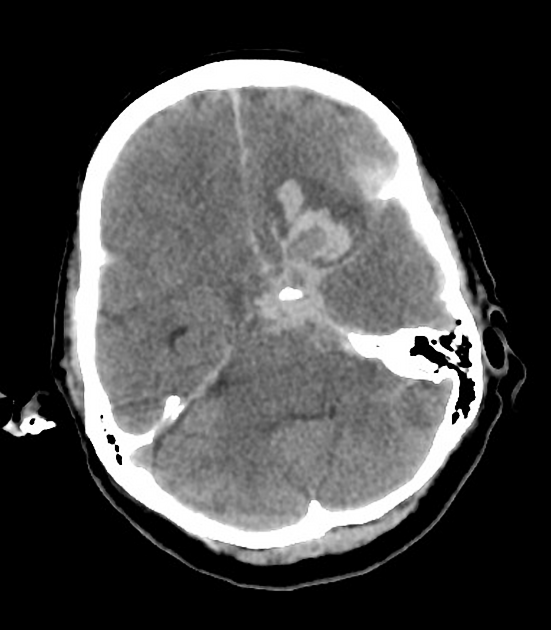
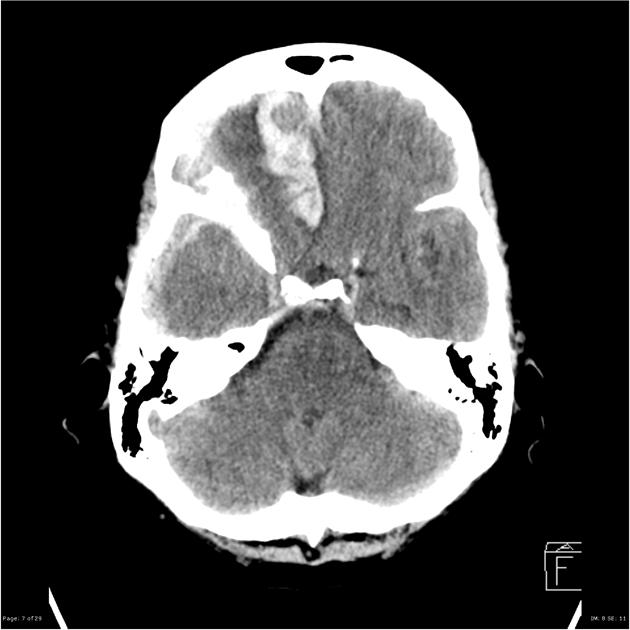
Radiographic features
CT
elongated hyperdense haematoma in the periphery of the affected lobe
the haematoma often 'points' to the site of the ruptured aneurysm
frequently associated regional or diffuse subarachnoid haemorrhage
may have associated subdural or intraventricular haemorrhage
the unthrombosed aneurysm may cause a "filling defect" within either the haematoma or adjacent subarachnoid haemorrhage
MRI
The appearance of haemorrhage on MRI varies with time and to some degree the size of the haematoma (see ageing blood on MRI).
Treatment and prognosis
Management is primarily of the underlying ruptured aneurysm or other vascular malformation. Otherwise, management of the intracerebral haemorrhage itself does not differ for other causes of intracerebral haemorrhage - please see the article on intracerebral haemorrhage for further discussion 7.
Differential diagnosis
In addition to aneurysms and other high-flow vascular malformations, the differential includes other causes of intraparenchymal haemorrhages including:
primary lobar haemorrhage or hypertensive haemorrhage (depending on location)
underlying tumours (metastases or primary tumours)
trauma (cerebral contusions)






 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.