Knee radiographs are common and often a quick and easy diagnostic exam in the emergency setting. An efficient approach to them requires a good understanding of anatomy with review strategies to ensure an accurate diagnosis.
On this page:
Systematic review
Choosing a search strategy and utilising it consistently is a helpful method to overcome common errors seen in diagnostic radiology. The order in which you interpret the radiograph is a personal preference. A recommended systematic checklist for reviewing musculoskeletal exams is: soft tissue areas, cortical margins, trabecular patterns, bony alignment, joint congruency, and review areas. Review the entire radiograph, regardless of perceived difficulty. Upon identifying an abnormality, do not cease the review, put it to the side and ensure to complete the checklist.
Soft tissue
Assess all soft tissue structures for any associated or incidental soft tissue signs. In the case of the knee, it will involve the detection of secondary signs such as effusion or soft tissue swelling.
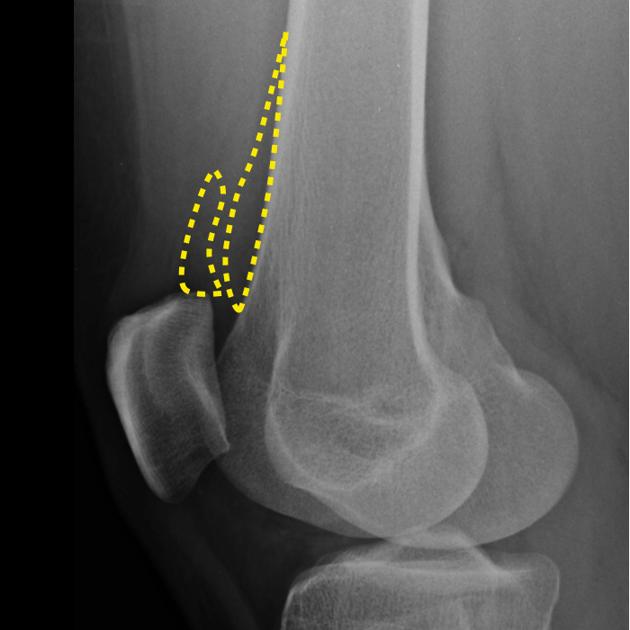
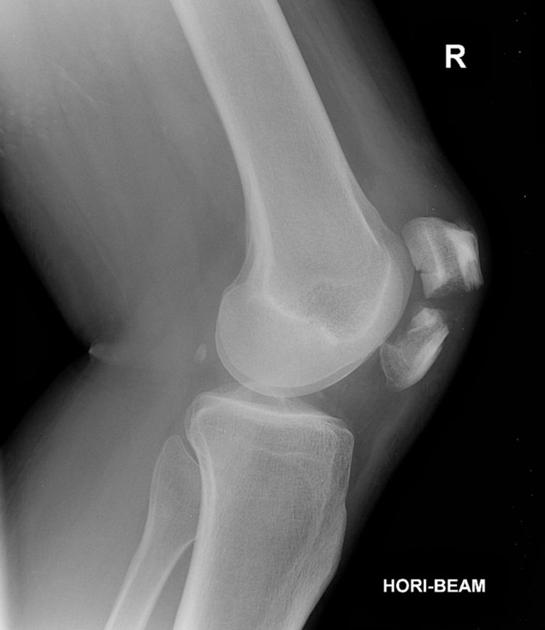
Check for an effusion on the horizontal beam lateral:
-
peripatellar fat pads should sit next to each other
-
soft tissue density between them indicates an effusion
if simple effusion (haemarthrosis), think of severe ligamentous, meniscal or intra-articular bony injury
if fat-fluid level (lipohaemarthrosis), think of an intra-articular fracture
Bone cortex
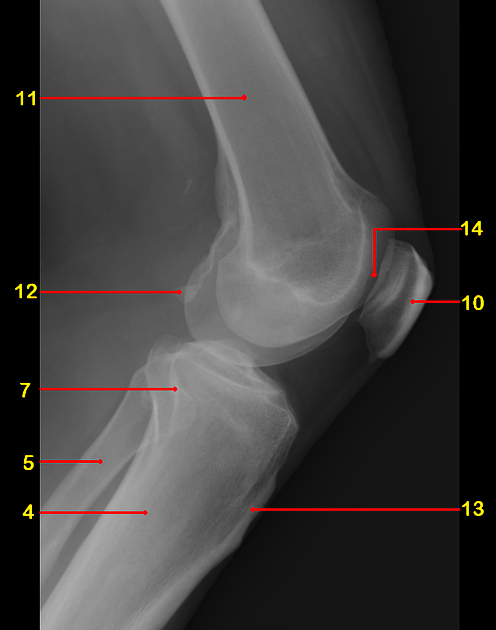
Trace the cortex of each bone paying particular attention to regions that are superimposed such as the fibular head or patella.
Plateau review
carefully look for a proximal tibial fracture
-
pay particular attention to:
tibial spine: avulsion
lateral tibial plateau: small avulsion (Segond fracture)
areas of increased density may point to underlying fracture
medial epicondyle: don't overcall calcification adjacent to the medial femoral epicondyle (Pellegrini-Stieda lesion)
Patella
fractures are usually easy to spot, often transverse
don't call a bipartite patella or tripartite patella fractures: well-corticated unfused centre(s) at the superolateral pole
Femoral condyles
-
subtle avulsion fractures can be hard to spot ensure to check the origins of the:
trace the articular surface keeping in mind the chance of an osteochondral defect
Bony alignment and joint congruency
One should inspect for smooth, concurrent bony alignment in all views.
-
tibiofemoral alignment
draw a line down the lateral margin of the lateral femoral condyle
if >5 mm tibia is observed outside the line, think tibial plateau fracture
-
check for patella tendon disruption
patella tendon: inferior pole of patella to tibial tuberosity
-
patella tendon length = patella length ± 20%
-
there are multiple techniques to measure this
-
if increased, think patella tendon rupture
Review areas
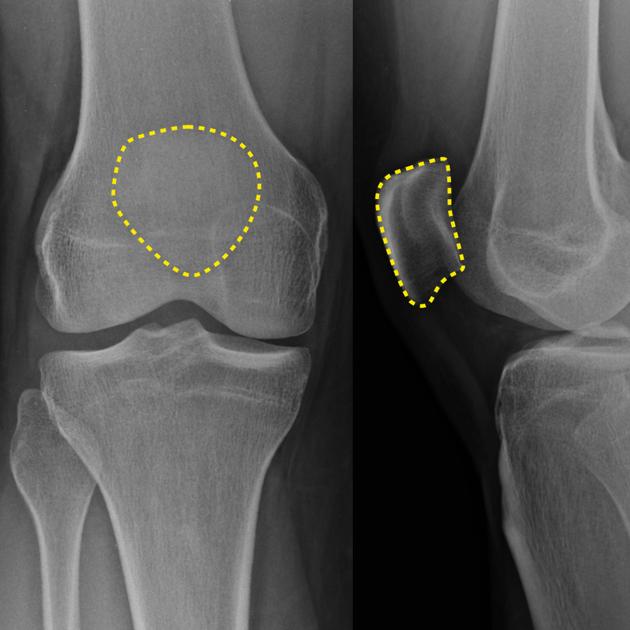
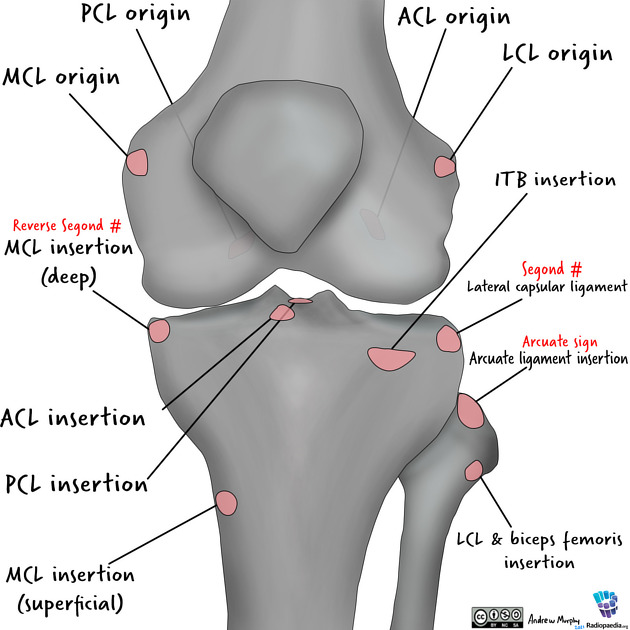
Small avulsion fractures of the knee more often than not are associated with instability and internal derangement. Careful scrutinisation of the origins and insertion points of ligaments is a must. From lateral to medial, superior to inferior, ensure to inspect 1:
origin of the lateral collateral ligament at the lateral femoral condyle
origin of the anterior cruciate ligament at the posterior-lateral portion of the intercondylar notch femoral condyle
insertion of the lateral capsule at the lateral tibia (at the joint line)
insertion of the arcuate ligament at the fibular styloid
insertion of the lateral collateral ligament and the bicep femoris tendon (conjoint tendon) at the fibular head
insertion of the iliotibial band at Gerdy tubercle of the tibia
origin of the medial collateral ligament at the medial femoral condyle
origin of the posterior cruciate ligament at the anterior middle portion of the medial condyle
insertion of the deep meniscofemoral ligament of the medial collateral ligament at the medial tibia (at the joint line)
insertion of the superficial fibres of the medial collateral ligament at the anteromedial tibia 5 cm distal to the tibiofemoral joint
anterior cruciate ligament insertion at the medial portion of the tibial spine
posterior cruciate ligament insertion at the posterior medial portion of the tibial plateau
It is worth spending extra time scrutinising areas of superimposition such as the fibular head and patella.
Common pathology
Lipohaemarthrosis
fat and blood from bone marrow collect in suprapatellar bursa
a fat-fluid level may be the only sign of intra-articular fracture
associated with tibial plateau or distal femoral fractures
more: lipohaemarthrosis
Tibial plateau fracture
80% involve the lateral plateau
fall from height or car bumper impact
associated significant cruciate and medial collateral ligament damage
more: tibial plateau fracture
Segond fracture
avulsion fracture; bony fragment adjacent to lateral tibial plateau
internal rotation and varus stress; falls or sports
75% associated with anterior cruciate ligament injury
more: Segond fracture
Intercondylar eminence fracture
typically avulsion fracture of tibial attachment of anterior cruciate ligament
mechanism: rapid deceleration or hyperextension of the knee
most common in adolescents
Patella fracture
majority transverse, also vertical or comminuted
direct blunt force or violent contraction of quadriceps
oblique or skyline views will confirm fractures
more: patella fracture
Distal femoral fracture
6% of all femur fractures
bimodal distribution
high energy blunt trauma; falls in elderly
more: distal femoral fracture
Proximal fibula fracture
typically occur with lateral tibial plateau fractures, but may be isolated
varus force
associated with lateral collateral ligament damage
more: proximal fibula fracture
Don't miss...
Pellegrini-Stieda lesion
post-traumatic soft-tissue calcification adjacent to medial epicondyle of femur
ossification following injury to medial collateral ligament
do not misdiagnose as a fracture
more: Pellegrini-Stieda lesion














 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.