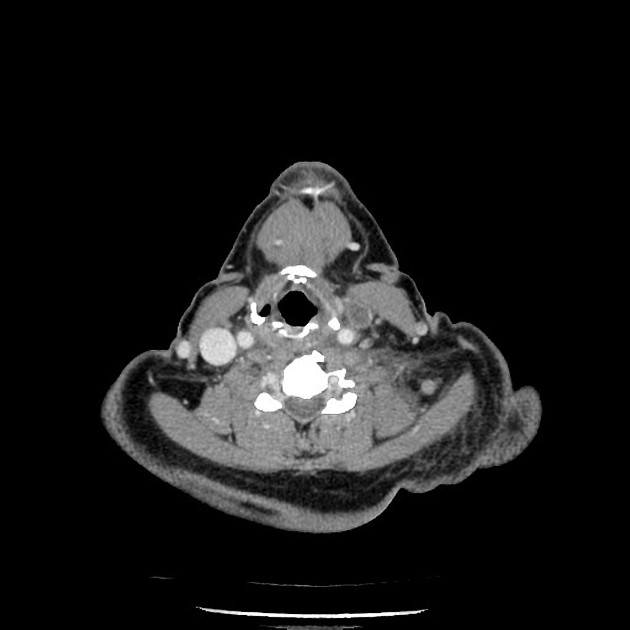
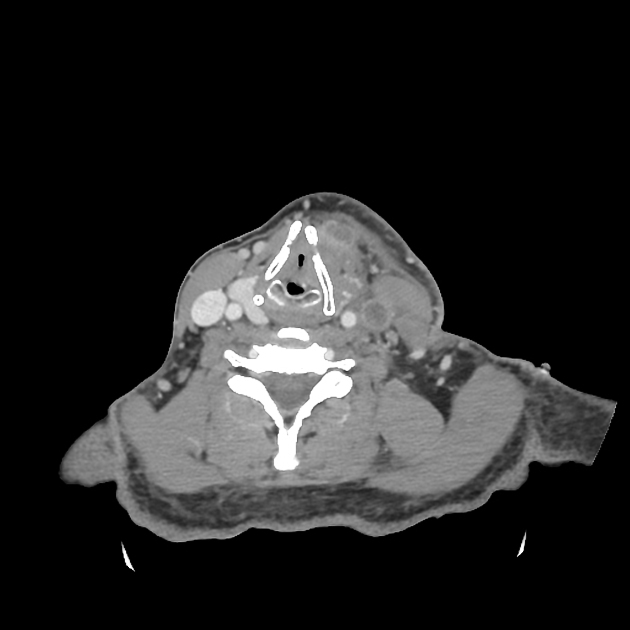
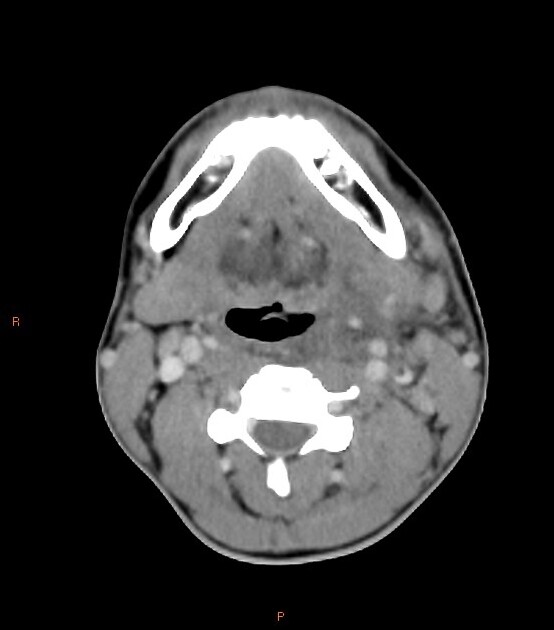
Lemierre syndrome, also known as postanginal septicaemia, refers to thrombophlebitis of the internal jugular vein(s) with distant metastatic anaerobic septicaemia in the setting of initial bacterial oropharyngeal infection such as pharyngitis/tonsillitis into lateral pharyngeal spaces of the neck with or without peritonsillar or retropharyngeal abscess. Diagnosis is made on the basis of clinical, microbiological and radiological investigations.
On this page:
Epidemiology
Since the advent of antibiotics, the incidence of Lemierre syndrome has reduced significantly, now affecting between 0.6-2.3 per million people. Lemierre syndrome classically affects young, healthy individuals with 70% of patients between the ages of 16 and 25 years. There is a slight male predominance.
Clinical presentation
Lemierre syndrome typically develops 4-5 days following an episode of acute pharyngitis or less frequently after acute sinusitis, otitis, or dental infection. Patients typically present unwell, with trismus and pain behind the angle of the jaw. Neck swelling may be evident.
Bacteraemia and distal infective thromboembolism are common 4,8:
lungs (in ~90%): pulmonary septic emboli (most common), lung abscess, empyema
central nervous system: dural venous sinus thrombosis (up to 20%), meningitis (~3%), cerebral abscess (rare) 8
joints: septic arthritis (15-25%)
liver: liver abscess (rare)
Pathology
An anaerobic Gram-negative bacillus, Fusobacterium necrophorum, is responsible for a majority (80%) of cases Lemierre syndrome, and gives rise to the term necrobacillosis 1. Fusobacterium necrophorum is a commensal organism of the upper respiratory tract. In up to one-third of patients polymicrobial bacteraemia is demonstrated, and anaerobic streptococci and other miscellaneous gram-negative anaerobes are also found frequently 8. Reports contain meticillin-resistant S. aureus (MRSA) as well 9. The causative bacteria are thought to spread directly from pharyngitis in the peritonsillar space to nearby tonsillar and internal jugular veins with subsequent septic thrombophlebitis.
Radiographic features
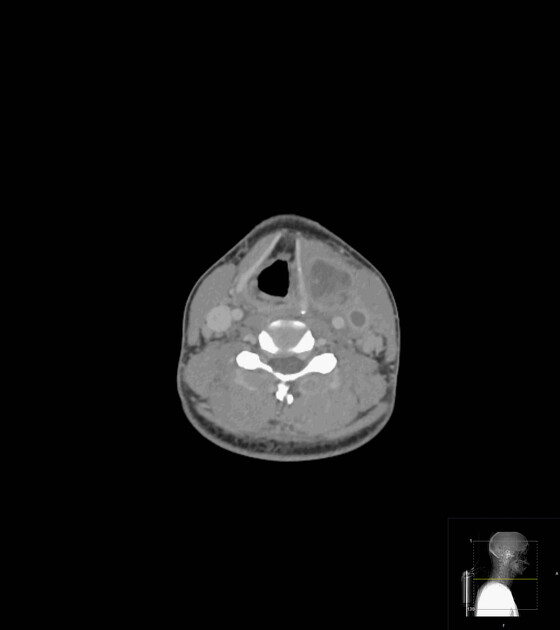
Radiological findings (such as internal jugular vein thrombophlebitis) often provide the first diagnostic clue, before bacterial cultures demonstrate positive growth. A high degree of suspicion in the appropriate clinical setting is essential for diagnosis.
Contrast-enhanced CT is considered the gold standard. Cases with isolated thrombophlebitis of tributaries of the internal jugular vein, e.g. common facial vein, have been described 2.
Ultrasound
Ultrasound may show hyperechoic thrombus within the internal jugular vein or other neck or facial veins. Spectral Doppler of a patent vessel may show loss of respiratory phasicity and cardiac pulsatility. This indicates the presence of a more proximal thrombus not accessible sonographically. The limitations of grey-scale ultrasound are well-described in the literature. Imaging with colour Doppler may overcome some of these shortcomings. The underlying site of infection is frequently not depicted.
Nonetheless, the identification of thrombophlebitis of the internal jugular vein is the first hard evidence to suggest Lemierre syndrome in many patients 8.
CT/MRI
Many authors consider CECT as the imaging study of choice due to its availability and its allowance for the visualisation of complications and underlying infection 6-8. Both modalities may with a high grade of confidence:
-
show an intraluminal filling defect in the jugular venous wall, frequently superior to ultrasound due to better assessment of deeper venous segments
also able to demonstrate complications such as dural venous sinus thrombosis
depict sites of septic emboli, most often encountered as pulmonary septic emboli (most commonly, see above), more readily visualised by CT
depict the site of primary infection
Treatment and prognosis
If unrecognised and untreated, systemic dissemination can occur with a dismal prognosis; studies from the modern era still report mortality rates as high as 18% 8. Treatment is usually with intravenous antibiotics and potentially surgical drainage for non-resolving abscesses 12. Anticoagulation may be used on a case-by-case basis, especially if there is evidence of dural venous sinus thrombosis 12.
History and etymology
It is named after Andre Lemierre (1875–1956) 11, a French bacteriologist who described the typical features of the disease in 1936 based on a case series of 20 patients 3. However Courmont and Cade first described the condition in 1900 as "human necrobacillosis" 11.
Differential diagnosis
isolated oropharyngeal infection
isolated jugular vein thrombosis
cervical lymphadenitis
pneumonia or metastatic disease







 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.