Leptomeningeal metastases, also known as carcinomatous meningitis and meningeal carcinomatosis, refers to the spread of malignant cells through the CSF space. These cells can originate from primary CNS tumours (e.g. in the form of drop metastases), as well as from distant tumours that have metastasised via haematogenous spread.
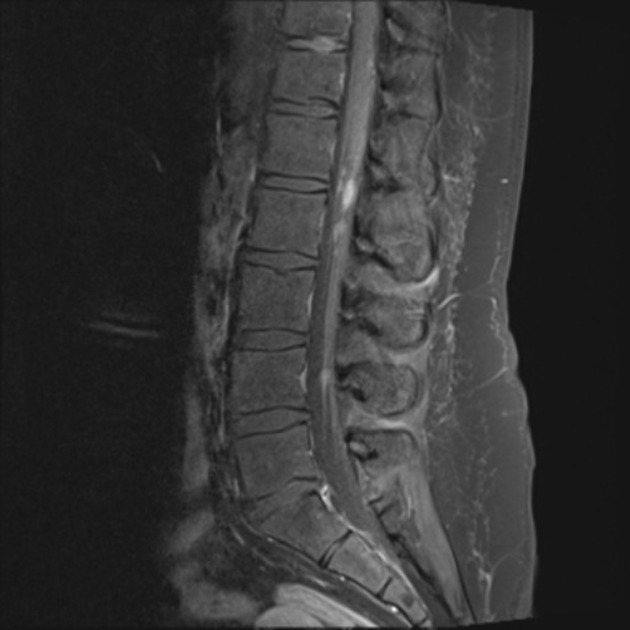
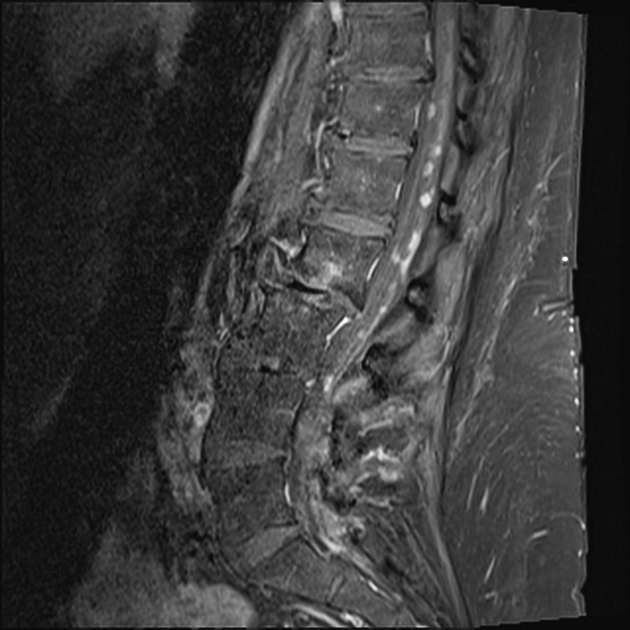
This article has a focus on subarachnoid space involvement. Refer to intradural extramedullary metastases for a discussion of leptomeningeal metastases in the spine. For other intracranial metastatic locations, please refer to the main article on intracranial metastases.
On this page:
Epidemiology
The demographics follow those of the underlying malignancy. Meningeal metastases were found in 8% of patients with metastatic cancer in cadaveric studies 22.
Clinical presentation
Clinical presentation is varied, but most commonly includes headache, encephalopathy, nausea and vomiting, and/or progressive multifocal neurological deficits (e.g. multiple cranial neuropathies and radiculopathies, myelopathy) 3. Meningism is only present in a minority of patients (13% 3).
Pathology
The primary intracranial malignancies that may cause metastases to the subarachnoid space are:
The vast majority of leptomeningeal metastases occur in the context of widespread metastatic disease, likely by haematogenous spread. Over 50% of cases have concurrent brain (parenchymal) metastases 13. The most common primary sites are:
breast cancer (particularly infiltrating lobular carcinoma)
gastrointestinal (e.g. gastric carcinoma 4,5, colorectal cancer 8)
haematological: lymphoma/leukaemia (leptomeningeal lymphomatosis)
Less common reported primary sites include:
intradural malignant peripheral nerve sheath tumour (MPNST) 18
cholangiocarcinoma (extremely rare) 21
Radiographic features
MRI
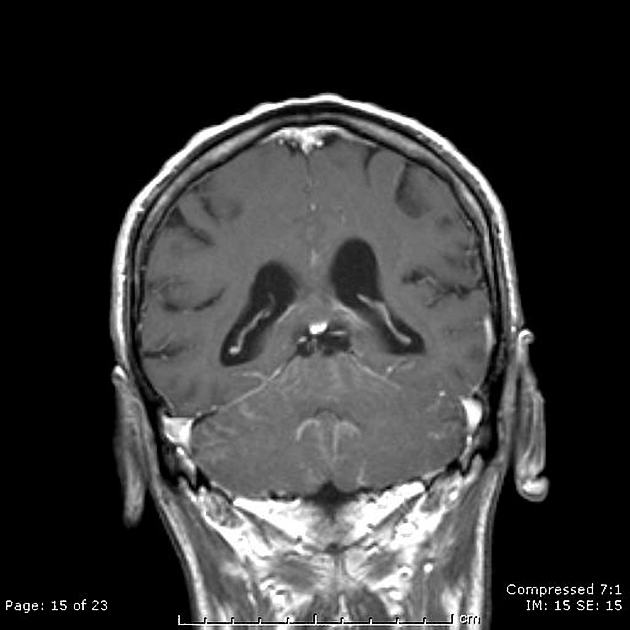
T1: usually normal
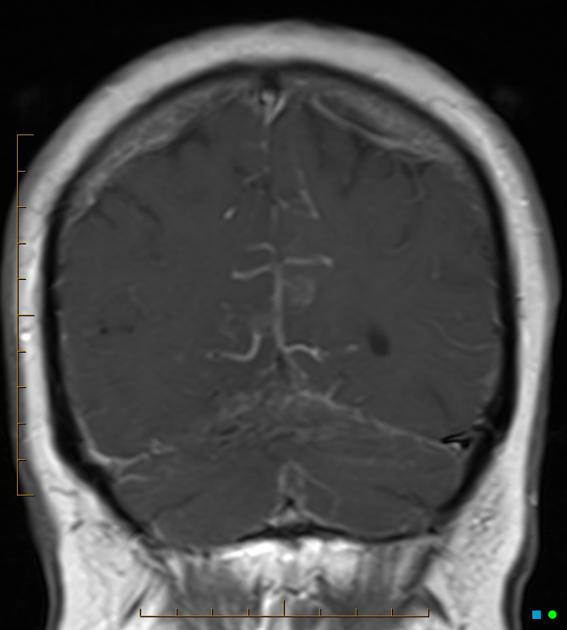
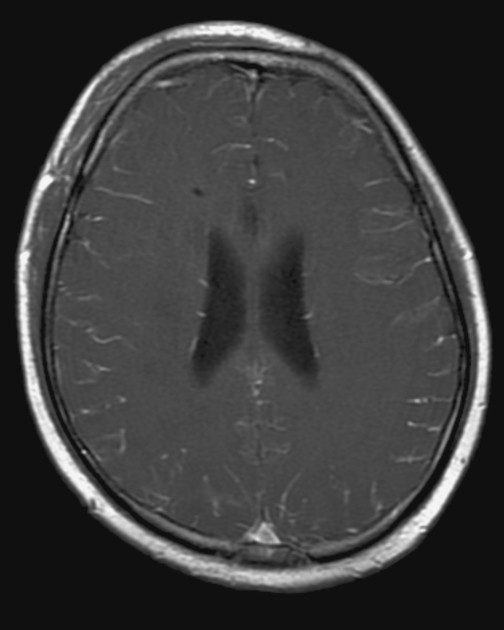
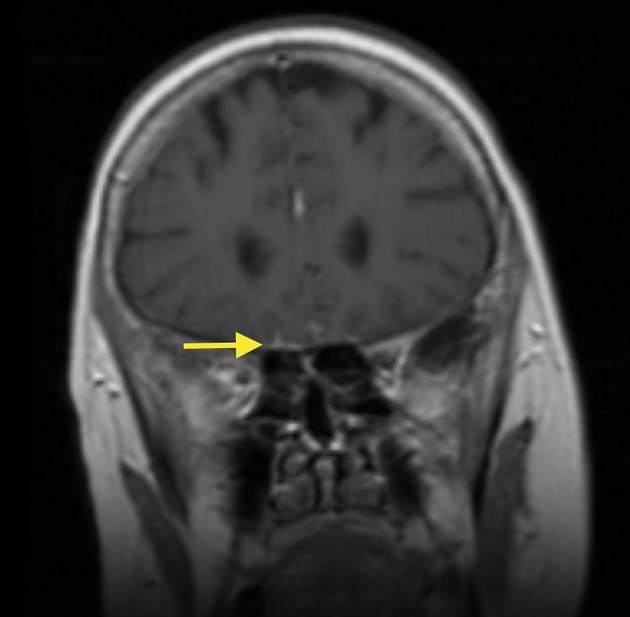
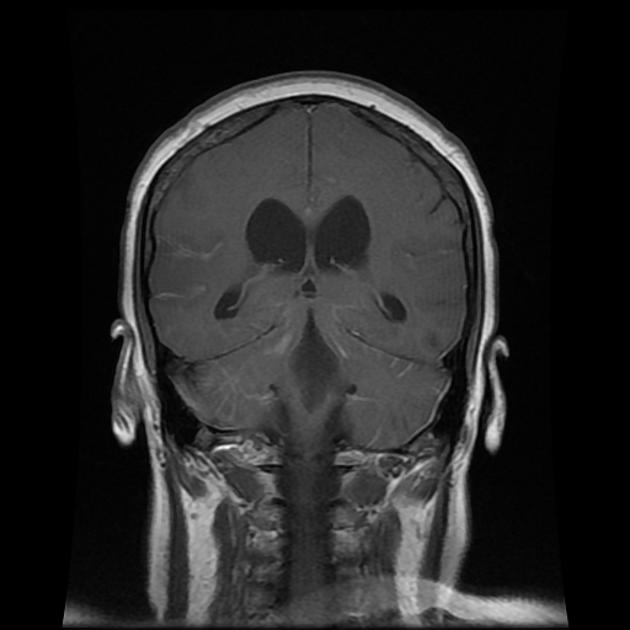
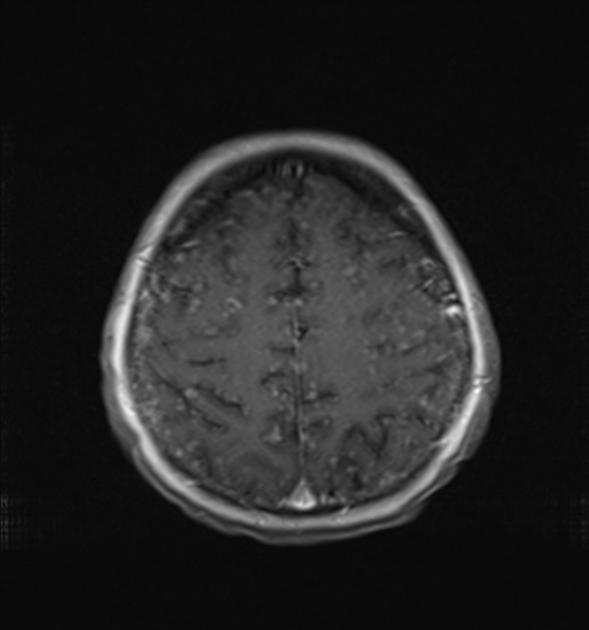
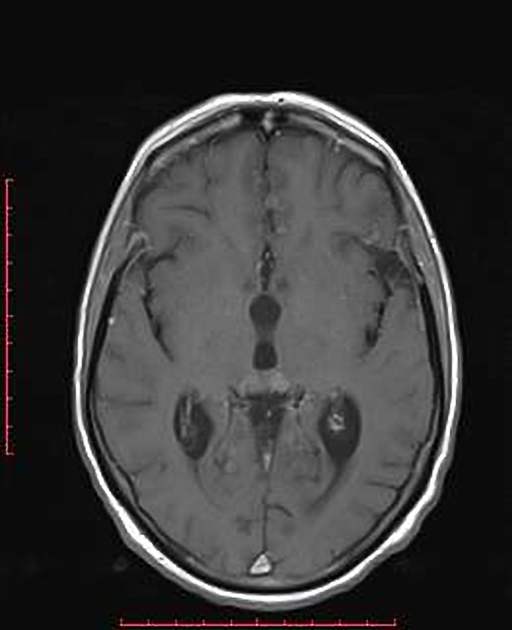
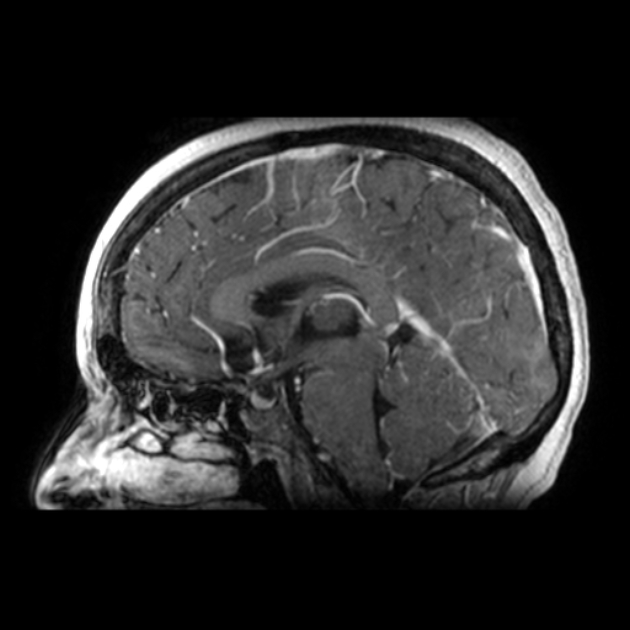
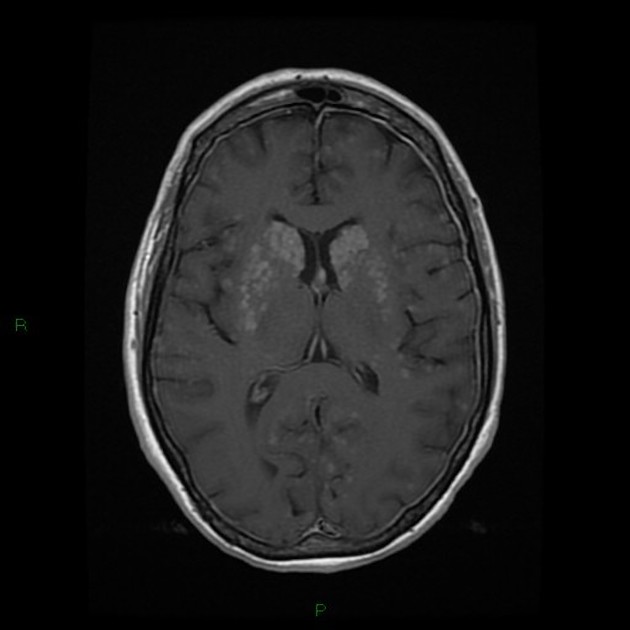
T1 C+ (Gd): leptomeningeal enhancement is the primary mode of diagnosis, often scattered over the brain in a 'sugar coated' manner
T2: usually normal; may show hyperintensity (including the bloomy rind sign in the brainstem 23)
-
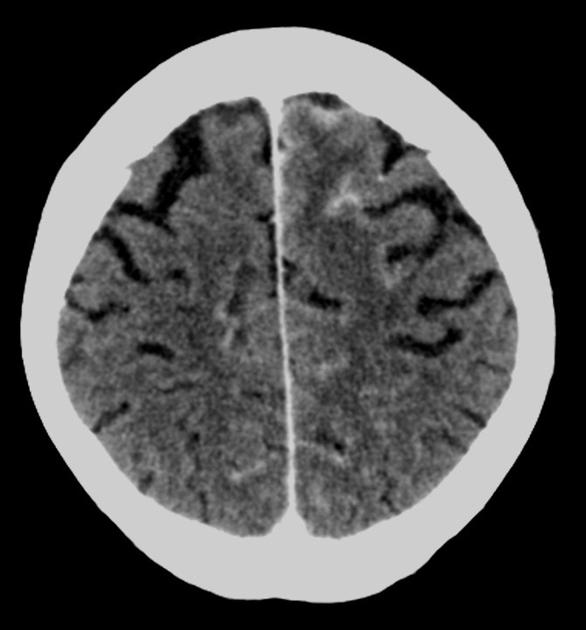
FLAIR
abnormally elevated signal within sulci 2 and rarely within the parenchymal surface (including the bloomy rind sign in the brainstem 23)
can be performed both non-contrast and post-contrast but is slightly less specific if performed post-contrast 1
Treatment and prognosis
Leptomeningeal metastases have a poor prognosis with patients usually succumbing within a few months (median overall survival 2.4 months 13). Treatment may extend survival to 6-10 months 2,3. Treatment can consist of 3:
intrathecal chemotherapy
radiotherapy
Resection is usually inappropriate due to the presence of widespread metastases at the time of diagnosis.
Differential diagnosis
slow flow in vessels
other causes of subarachnoid FLAIR hyperintensity






 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.